
Expired activity
Please go to the PowerPak
homepage and select a course.
Pediatric Readiness in the Hospital Setting: Preparing Pharmacists for Pediatric Emergencies
INTRODUCTION
Disasters of one type or another are a common occurrence in the world today. Local and
national media document the events from whatever part of the globe they are occurring.
The result is increased sensitization and awareness of the general population to these
threats and their devastating impact. Disasters can affect individuals, families, and sadly, children. Victims and witnesses to
the devastation frequently struggle with disaster reactions and recovery. Health care
providers who see and hear about disaster often try to imagine how they would handle
similar disasters, and when children are involved, their empathy and compassion is part
of their reaction. Those who have worked in disaster response can educate pharmacists
about pediatric readiness with a critical piece of advice: Preparation promotes resiliency.
THE CHANGING FACE OF DISASTERS
When we think of disasters, most of us tend to think of weather-related and high-profile
events such as tornadoes, plane crashes or fires. Disasters, however, come in a large
variety of types. The International Federation of Red Cross and Red Crescent Societies
(IFRC) define a disaster as "a sudden, calamitous event that seriously disrupts the
functioning of a community or society and causes human, material and economic or
environmental losses that exceed the community's or society's ability to cope using its
own resources."1
Vulnerability
Unanticipated, threatening events of equally apparent magnitude that occur in different
places can have vastly different consequences. The IFRC uses a mathematical equation to
explain how an event that is inconvenient or temporarily stagnating in one place becomes
a disaster in another1:
(vulnerability + hazard)/capacity = disaster
Vulnerability-the diminished capacity to anticipate, cope with, resist and recover from the impact of a natural or man-made hazard-changes with time and situation. Poverty is a
primary contributor to vulnerability. An example of vulnerability is a common problem in many areas: poorly constructed or maintained housing in low-income areas will not
withstand hurricane winds or floods as well as better (and more costly) housing. However,
isolation, insecurity, and defenselessness also influence vulnerability. Thus, physical,
economic, social, and political factors determine vulnerability.1
Hazards are just what they seem: natural or manmade occurrences that create danger.1
Capacity is preparedness: measures taken to prepare for and reduce any disaster's impact.
The health care system is a critical component of capacity.1
Children and Disaster
Who are your community's most vulnerable and has your health care system and
community planned for them? People who are isolated, such as older patients, or those
who are defenseless, such as the chronically ill or hospitalized, need extra help during disasters. Here we discuss a third group-children who are dependent on others, have little
experience, and possess no resources of their own. This triad makes them insecure and
exceedingly vulnerable, yet many disaster plans focus mainly on adults.
Importance of Anticipating Children's Injuries
United States (U.S.) census data from 2014 estimate that children under the age of 5
years account for 6.2% of our population. A full 23.1% of our population is less than 18
years of age.2 Traditionally, disaster planners have considered children and to some
extent, adolescents, as primarily secondary victims-patients who are exposed to the
disaster but shielded by adults-and addressed children in proportion to their census
representation.
Perpetrators of terrorism in recent situations have victimized children intentionally to
create a greater psychological shock.3,4,5,6 Terrorist attacks may harm greater numbers of
children, and sometimes harm only children.3 Terrorists may plan concurrent multiple
attacks simultaneously to increase fear and bottleneck the first police, firefighters and
emergency medical technicians to arrive at the scene (first responders).3,7 This possibility
mandates careful planning in places where children dwell: home, schools and day care
centers.4
Disasters' changing nature should prompt health care systems to revisit their ideal surge
capacities (the ability to rapidly move from normal operation to a significantly higher
capacity) and antidote/treatment needs. Increasingly, surge capacity needs to anticipate
pediatric victims. Only 55% of all U.S. hospitals have children's beds, and only 5% of
adult hospitals have sufficient resources to manage a broad range of pediatric needs. This
raises unique concerns about resources.3,7
Preparing in Advance
Local hospitals generally hold annual disaster training drills, tabletop exercises, or mock
disasters (see Table 1). These drills, required by the Joint Commission and other
accrediting and certifying organizations, are designed to promote teamwork skills in
high-stress disaster environments. They focus on improving health care team members'
communication and collaboration, and also teach team members to "suspend disbelief."
| Table 1. Preparedness Exercises for Health Care Systems and Communities |
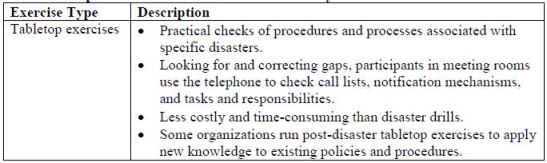
 |
| Source: References 8 and 9 |
Samuel Taylor Coleridge coined the term "suspend belief" 200 years ago. Originally it
meant appreciating literary or dramatic works that explore events or characters that would
ordinarily be considered implausible. It's been adapted in disasters to mean put aside
emotions and preconceived notions and temporarily accept the new reality. Those
involved in triaging children at the scene or in the hospital may be unfamiliar with
children in general or pediatric medicine specifically, or may be overly empathic in
situations where the child may die from his or her exposure.10
Often, hospitals and health care systems either overlook or under-represent pediatric
patients in disaster planning. They fail to acknowledge how children will affect surge
capacity and may underestimate health care providers' emotional stress (and difficulty
suspending disbelief) when an event harms children.6
DISASTER TEAMS/GOVERNMENT RESOURCES
The federal government establishes the disaster response structure that state and
communities entities follow, and it influences every health care system's specific disaster
response protocols. The U.S. Department of Homeland Security (DHS) is responsible for
thwarting terrorist plans and ensuring preparedness for such attacks and appropriate
response to those events.3
The Federal Emergency Management Agency (FEMA) was initially created in 1978 and
is now part of DHS. Working out of 10 regions, FEMA staff members coordinate actions
and respond to homeland disasters when local and state resources have been exhausted.3
Disaster Medical Assistance Teams (DMAT) are groups of health care providers and
support personnel, including pharmacists. DMATs can be activated for a period of 2
weeks. DMAT teams provide rapid-response medical care to disaster areas. Once
deployed, they bring supplies and equipment to sustain their mission for up to 72 hours.
Their responsibilities include triaging and medically managing critically ill patients in
inhospitable environments. DMATs currently have no pediatric requirements for team
members, and the teams carry limited pharmaceuticals and equipment for children. In the
U.S., 2 pediatric teams exist; however, they are self-certified. 3,11,12
The Medical Reserve Corps (MRC) includes groups of public health and medical
volunteers dedicated to their communities' health and safety. They prepare for natural
disasters and other unanticipated emergencies that affect public health. They have no
clear pediatric capabilities in disasters, nor is pediatric readiness an MRC requirement.3
Congress established the CDC's Strategic National Stockpile (SNS) in 1999. Its mission is to resupply essential medical supplies and equipment needs during emergency disasters.
States and communities can tap into the SNS within 12 hours of exhausting local caches
once the federal government approves the community for assistance. SNS provides U.S.
Food and Drug Administration (FDA)-approved antibiotics, antidotes/antitoxins, airway
management supplies (e.g., ventilators, inhalers) and other medical and surgical supplies
free of charge. The CDC SNS staff members deploy a "push package" first that includes a wide range of pharmaceuticals, antidotes, and supplies intended to cover unknown
disasters. The SNS stores these push packages regionally to permit deployment within 12
hours of federal approval. Once area health and safety personnel define an incident and
supplies dwindle, contracted distribution centers ship vendor-managed inventory (VMI)
within 24 to 36 hours with supplies and pharmaceuticals more specific to the
exposure/event. The SNS's utility in caring for pediatric disaster victims is limited
because many antidotes/antitoxins used in pediatric care are not FDA-approved.3
PEDIATRIC PATIENTS: NOT SMALL ADULTS
In addition to understanding the emergency response system, pharmacists need to
understand some basics of pediatric care. Pediatric patients' vulnerability stems from their
physiologic and psychological immaturity, which significantly increases mortality risk.
Developmental Considerations
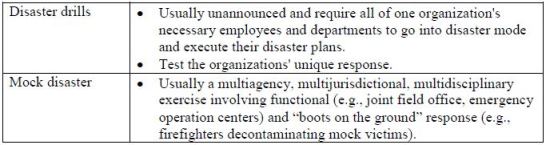
Pediatric patients' development is immature, and their systems differ from those of adults
in important ways (see Table 2). Most health care providers are aware of pediatric
patients' predisposition to gastrointestinal distress. Children are highly susceptible to
dehydration due to nausea, vomiting, and diarrhea. Clinicians may be unaware that
vascular access is likely to be a problem with smaller children. They need to know about
intraosseous infusion (injecting directly into bone marrow to provide a noncollapsible
entry point into the systemic venous system). In addition, children can be quite thin or
obese, and some health care providers are unfamiliar with autoinjector devices (i.e.,
atropine, epinephrine, pralidoxime chloride).3,6,13
Heightened awareness of needle length, dose, and the actual injection process ensures
successful use. The autoinjector's needle may be too long for thin children, and too short
for obese children. Atropine and pralidoxime autoinjectors formulated for adults deliver
doses too large for infants and children, although children often tolerate atropine
overdose. Children symptomatic from nerve agent poisoning will likely need both
supraphysiologic doses and frequent redosing of atropine. Human factors also interfere with drug efficacy. Unlike regular injections, some
autoinjectors are not designed for jab and pull administration, and need to rest in place on
the patients skin for several seconds.14-16
| Table 2. Children's Unique Characteristics |
 |
| Source: References 3, 7, 13, and 17 |
In essence, "The smaller the child, the bigger the problem regarding any of these
considerations such as hypothermia, airway management, separation of family, and
ability to effectively decontaminate the child."13
Collateral Concerns
Acute injury is just one consideration when children are harmed in disasters. Exposure to
toxins, carcinogens, and radiation can damage DNA and predispose children to cancer at
later time points; good documentation in children's medical records is critical.3,6,13 Other
concerns include making every attempt possible to keep families together, and if not,
reuniting pediatric patients with family members as soon as possible. This can be a
challenge.
IDENTIFYING AND TRIAGING PATIENTS
The CDC developed the mnemonic, SALT (Sort, Assess, Lifesaving Interventions,
Treatment/Transport) to channel patient triage in times of a mass casualty. It is useful in
all populations. When triaging pediatric patients, health care providers must emphasize to
airway assessment, as children are more likely to experience respiratory arrest than adults
(who are more likely to have cardiac arrest). SALT's goal is appropriate transport and
rapid treatment with the correct decontamination, antidotes, and supportive care
measures.10
Clinicians need to be cognizant of pediatric patients' unique psychological needs. Their
physical symptoms (abdominal pain, headache) may actually be manifestations of stress
or anxiety. Disasters themselves cause stress and anxiety, but health care settings do, too.
Children have limited to no understanding of the health care system. Clinicians can
reduce children's stress by taking these steps18:
• Minimizing painful and/or invasive procedures
• Discussing procedures before starting so children will know what to expect
• Educating children in an age-appropriate way about their injuries or illnesses
• Asking parents to coach and soothe the patient
• Having activities (coloring books, toys, television) to redirect children's attention during waiting times
Stress may also worsen pre-existing disease, such as an increase in blood glucose for
those with diabetes or worsening of asthma symptoms.19
Types of Threats
Some disasters are seasonal variants (e.g., tornados, hurricanes, floods). Though often
caused by nature, disasters can and often do have human origins. Manmade disasters can
include bridge failures, accidental industrial explosions, transportation disasters, and
other unanticipated events. In recent years, thoroughly unpredictable terrorist attacks
have challenged the disaster response system and created a need for health care providers
to familiarize themselves with the weapons that terrorists use.3
Natural Disasters
The majority presidentially declared disasters (90%) are weather-related. Cornell
University Cooperative Extension Service notes that weather-related and natural disasters
seem to occur more frequently lately and result in greater devastation. Presidentially
declared disasters cause an average of 500 deaths and $14 billion in damage annually.20 Meteorologists can predict many weather-related events, while others such as
earthquakes and tsunamis occur randomly. Regardless, the ensuing damage depends on
many variables. Adequate public warning systems, heightened awareness and appropriate
actions-that is, planning, preparation, and following through with appropriate and timely
action-make huge differences in the aftermath.
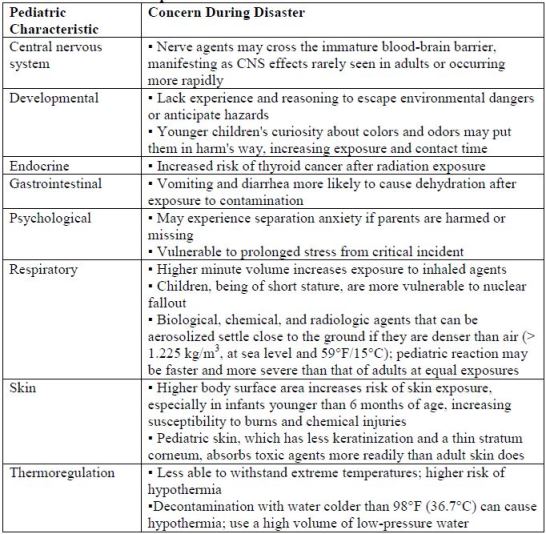
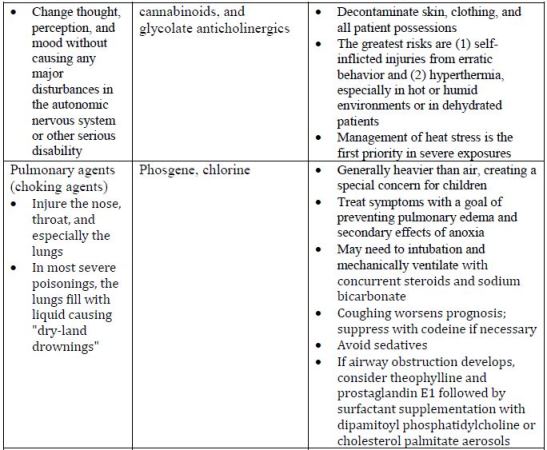
Natural disasters come in many forms, and create concerns about injury and illness, food
and water safety, environmental concerns including mold, and animal (rodents, snakes,
and stray dogs) and insect (mosquitoes and ticks) hazards. Table 3 describes events that
often lead to widespread disaster. Of note, when traumatic injury is possible, some
researchers now recommend using personal protective devices including infant car seats
and helmets inside the house to protect children.21
| Table 3. Natural Disasters and Health Care Concerns |
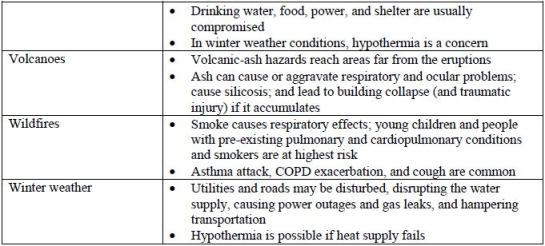 |
| Source: References 21-28 |
Natural disasters can injure people who remain in the area or displace victims from their
homes. Both often occur. This challenges health care systems, and especially emergency
departments, in the disaster area and in communities that accept evacuees. Emergency
departments often experience overcrowding as people harmed in the disaster seek
emergency care and in areas that have extensive damage, need to replace the supply of
medications for chronic diseases. Evacuees often forget or lose their medications as they
flee the disaster. Faced with temporary relocation, they seek care for emergency and
routine problems such as prescription refills in urgent care and emergency departments
because they have no local primary care relationships. The jurisdictions' mobile units and
county public health employees are sent to help.29
A significant concern in the aftermath of natural disasters is carbon monoxide poisoning,
which causes headache, dizziness, weakness, nausea, vomiting, sleepiness, confusion,
and ultimately death. Gasoline-powered generators release carbon monoxide. People who
use gasoline-powered generators for energy need to be reminded to install them correctly
and away from their homes. They must not use generators, charcoal or gas grills, gas
lanterns, or camping stoves in enclosed areas, nor should they use ovens as heat
sources.24
Biological Agents
• Biological agents have the potential to kill or maim large numbers of people very
quickly, and are a leading concern among disaster response agencies. Methods
that aerosolization or mass dispersion of bacterial agents create considerable
concern. Children are likely to be most vulnerable to these biologics due to their
unique physiology. Pathogenic biological agents affect the child through
production of toxins and/or host cell invasion.
Exposure to many of these agents causes an initially mild prodrome. The pediatric patient
typically presents with nondescript complaints of fever, chills, headache, nausea,
vomiting, and/or diarrhea. Differential diagnosis (i.e., is the problem a typical pediatric
viral illness or exposure to a toxin?) is difficult. Further, very young patients lack
language skills to describe their symptoms effectively.
Biological agents are classified as Class A, B, or C (Table 4). Anthrax, botulinin toxin,
plague, smallpox, tularemia, and viral hemorrhagic fevers are the greatest public health
risks.30
| Table 4. Biological Agents by Class |
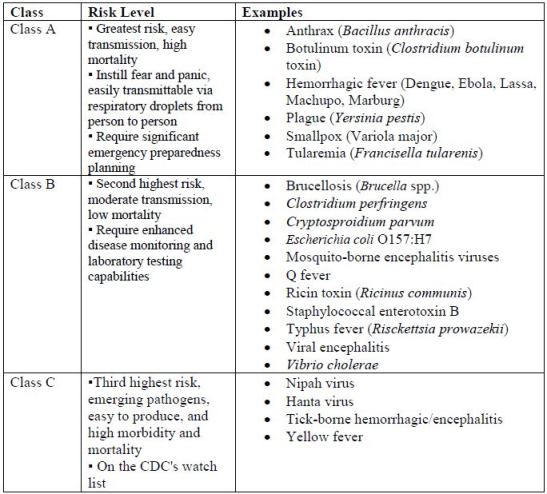 |
| Source: 30 |
The first step in responding to a known biological attack is addressing the health
system/hospital's triage needs. Practitioners must be prepared not only for the exposed
and sick children but for the worried well. Determining the need for isolation and
quarantining exposed patients is necessary to protect nonexposed patients and health care
staff. Decontamination methods must also be evaluated.31
The next step is addressing the specific agent. Many different antibacterial agents exist,
but pediatric dosing, dosage formulations, and FDA approval may be lacking or
challenging. Treatment dosing differs from prophylaxis dosing. Since 1969, the U.S.
Army Medical Research Institute of Infectious Diseases (USAMRIID) has prepared and
updated a resource that addresses mass dispensing. Available online, it includes treatment
doses, prophylaxis doses, and vaccination information along with monitoring perimeters
for affected individuals.31
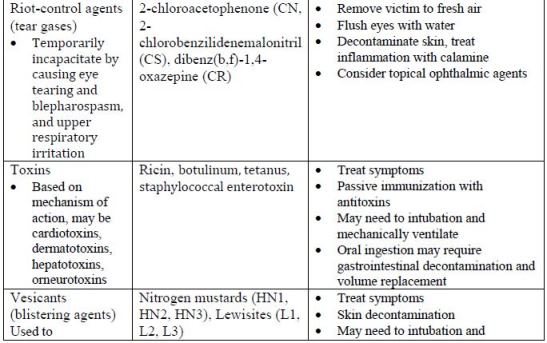
Chemical Agents
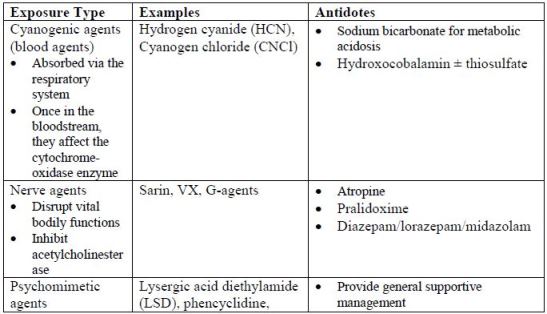
Chemical agents-called weapons of mass destruction (WMD) because they can kill
hundreds of people quickly-have been used in many wars (see Table 5). They tend to be
inexpensive, easy to obtain, and generate more fear than either biological and/or
radiological terrorism. Small amounts dispersed as gases, liquids, or aerosolized agents
can create mass causalities.32
| Table 5. Weapons of Mass Destruction32-34 |
 |
When terrorists use chemical agents, patients develop signs and symptoms quickly but
first responders and health care providers may not be able to determine the specific agent
immediately; symptoms, onset, and latency overlap and vary considerably among
agents.34 Treatment is twofold: evacuating the affected area followed by rapid
decontamination.
First responders and public health officials identify the event's "hot zone" (the area
considered to be in greatest danger) to help with triage and treatment needs.35Decontamination has 2 objectives: (1) to treat exposed individuals and (2) to minimize
the risk of health care providers experiencing secondary exposure (exposure via residues
on patients' clothing and belongings).32 As in many other areas of medicine, emergency
responders increasingly rely on mobile medical applications and identification/diagnostic
tools to identify the agent quickly, triage effectively, and access information quickly.34
Physical decontamination includes elimination of chemicals. It starts with removal and
sequestration of all clothing and accessories, followed by cleansing with soap and water,
or using adsorption with adsorbent agents (e.g., activated charcoal, kaolin, resin, talc). In
an emergent setting, responders could use available adsorbents (e.g., uncontaminated soil
or flour) as scrubbing agents in the decontamination process. The wash water and
adsorbent materials become contaminated and require their own specialized handling and
disposal.32
Another method of decontamination is to create a chemical reaction (nucleophilic or
oxidation reactions) that render the chemical weapon useless. When used appropriately,
this method is more effective than physical decontamination. Commercial
decontamination kits are available and may contain ethanol, phenol, sodium hydroxide,
ammonia, and water. Household bleach can be used as a skin decontaminant.32
Radiological Agents
Humans are exposed to low levels of radiation-called background radiation-from
sunlight, radon gas, and microwaves daily. In the United States, background radiation
accounts for about half of all human radiation exposure. Medical radiographs account for
the remaining usual dose, with a total average dose of 620 millirem (0.0062 Gy). Patients
who undergo radiation for cancer have exposures that are considerably larger than the
average American.36 Radiation levels can be troublesome in some natural disasters. An
example is the 2011 Fukuskima nuclear disaster, in which an earthquake and resulting
tsunami destroyed a nuclear power plant.37
Radiation is also employed by terrorists. Terrorists' dirty bombs spread low-grade
radioactive materials, creating more panic and fear than physical injury and exposure
after detonation. However, significant radiation exposure can occur, and the total
radiation dose, measured using biodosimetry tools developed for field and bedside use, is
the most reliable predicator of patient outcome.34,38 Foreign bodies imbedded in skin and
tissue also cause injuries.33,39
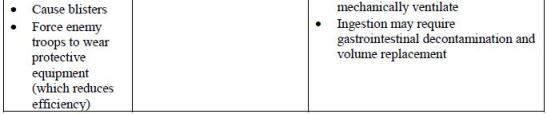
Acute radiation syndrome progresses through 4 phases (Table 6). Radiation doses that
exceed 2 Gy are most likely to cause acute radiation syndrome.36,40
| Table 6. Four Phases of Acute Radiation Syndrome |
 |
| Source: References 33 and 39 |
| Abbreviations used: CNS - central nervous system; G-CSF - granulocyte colony stimulating factor; GI - gastrointestinal; Gy -gray, unit to measure irradiation. 1 Gy = 100 rads; PRBC - packed red blood cells; rad - radiation absorbed dose. |
Public health officials act when radiation disasters occur. Actions range from advising
residents to remain indoors (sheltering in place) to evacuation, which minimize or
prevent radiation exposure. During Fukuskima nuclear disaster, the public health
response was swift. No radiation-related deaths occurred because of the rapid evacuation
of the affected area.37
Radioactive iodine-131, a fission product, is emitted in many nuclear disasters.
Administration of potassium iodide (KI) is a possible prophylactic agent or treatment.
Most effective when taken before exposure, KI blocks thyroid 100% of uptake of
radioactive iodine . It exerts its effects for up to 24 hours, making it an ideal prophylactic
agent for those near nuclear plants. After exposure, clinicians must give children KI
within 24 hours as its efficacy decreases dramatically to less than 10% after that.39 Experts recommend treating children more aggressively than adults, and administering
KI at an exposure threshold of 5 rem; adults are treated at 10 rem. KI is an appropriate
protective action only in radioactive iodine; it does not provide protection against other
radioactive substances.41,42
Pediatric patients, with their greater body surface area and poorly keratinized skin, are at
great risk for thermal and radiation burns. Small children are usually uneducated about
the need to shield their eyes from radiation sources (or incapable of doing so); this
increases risk of eye injuries as their lens is more sensitive to radiation damage from blast,
radiation, or thermal exposures.39
As with other agents, decontamination is an important first step in radiation containment.
Removal of the child's clothing, shoes, and accessories followed by double bagging can
contain up to 90% of the radiological agent. Cleaning and scrubbing with soap and water
removes radiological dust. All bodily fluids (blood, emesis, stool, urine) must be
considered contaminated and handled as toxic waste.39
Clinicians should draw blood and order complete blood counts 3 times daily for the first
2 to 3 days, watching for changes in the patient's lymphocyte counts.39 Several cytokines
can be employed to correct radiation-related myelosuppression, and they can be used in
children. The FDA has approved a filgrastim dose of 10 mcg/kg/day as a single dose in
children, with daily dosing until the absolute neutrophil count exceeds 1,000/mm3.
Pegylated filgrastim is also FDA-approved, and clinicians should refer to the approved
product labeling for pediatric dosing. The need for cytokines may far exceed their
availability, and because of this, U.S. Department of Health and Human Services
Radiation and Emergency Medical Management division provides an online triage
calculator to help health care providers determine which patients have the greatest need
based on exposure type and resultant laboratory values.41
Low-level radiation's psychological effects can linger for many years. Damage from
very-low-level radiation is undetectable; people who are exposed worry about long-term
effects or possible reproductive issues (so they avoid having children). They have also
been stigmatized by their communities.43,44
PHARMACIST OPPORTUNITIES
Mass casualties consume pediatric resources, quickly overwhelming systems. Developing
a pediatric-specific cache of medications and policies and procedures that address
handling, storage, expiration considerations (with rotating soon-to-expire drugs back into
hospital supplies), recipes for compounding oral solutions, compounding injectable
medications from bulk powders (atropine), and dosing guides, will prepare pharmacists to
be effective members of health care support disaster teams.3,45,46
Most communities need health care professionals including pharmacists to become more
involved in disaster planning. As drug experts, pharmacists who volunteer with hospital-based disaster teams and community planning can advocate for appropriate medications
and ongoing training. They can mentor and educate new pharmacists and help
experienced pharmacists maintain relevant skills. Training is the cornerstone of
preparation, and scheduling disaster drills and tabletop exercises that include pharmacists
and pharmacy technicians maintains essential skill sets.3,45,46
Protocols and order sets that are both online and in hard copy are essential. Pharmacy
involvement from design to implementation is important. Pharmacists can address
pediatric patients' unique characteristics and dosage concerns, thereby reducing risks.
Pharmacists need to be part of discussion on how to manage limited resources and be
familiar with ethical considerations and criteria for release to use on pediatric patients.
Understanding triage and decontamination needs will also help minimize pharmacist
and/or pharmacy technician risk of secondary exposure.3,45,46
During disasters, pharmacists in leadership roles and those with scheduling
responsibilities need to anticipate workforce problems. Studies have demonstrated up to
17% reduction in overall workforce during mass casualties. Health care employees, like
others in the area, have family and/or child care needs. That reality influences their
willingness and ability to respond to a disaster. Their families' and their own safety will
be another obstacle; employers who anticipate their needs will be best positioned to
help.3,45,46
SUMMARY
In times of disaster, pharmacists have unique roles, knowledge, and responsibilities. They
can ensure that hospitals and communities plan adequately for pediatric needs.
Pharmacists' advice about treatment plans, order sets, and procurement of necessary
pharmaceuticals and supplies is invaluable. In addition, all health care providers must
work with agencies outside their institutions to streamline those decision processes
regarding pharmaceuticals and identify new roles that advance pharmacy's mission and
vision.
References
1. The International Federation of Red Cross and Red Crescent Societies. What is a
disaster? Available at https://www.ifrc.org/en/what-we-do/disaster-management/about-disasters/what-is-a-disaster/. Accessed January 27, 2016.
2. United States Census Bureau. QuickFacts United States 2014. Available at
http://quickfacts.census.gov/qfd/states/00000.html. Accessed January 24, 2016.
3. Markenson D, Reynolds S. The pediatrician and disaster preparedness. Pediatrics. 2006;117(2):e340-e362.
4. Redlener I. Children as potential targets of terrorism. [Conference report].
http://ncdp.columbia.edu/custom-content/uploads/2015/01/REPORT_Children_Targets_Terrorism_06.pdf.
Accessed June 25 2015.
5. Burke RV, Iverson E, Goodue CJ, et al. Disaster and mass casualty events in the
pediatric population. Sem Ped Surg. 2010;19:265-270.
6. Dolan MA, Krug SE. Pediatric disaster preparedness in the wake of Katrina:
lessons to be learned. Clin Ped Emerg Med. 2006;7:59-66.
7. Abraham H. Planning for Pediatrics in Disasters. 2014
http://www.jems.com/articles/print/volume-39/issue-9/patient-care/planning-pediatrics-disasters.html Accessed Jun 15 2015.
8. Chandra A, Williams MV, Lopez C, Tang et al. Developing a tabletop exercise to
test community resilience: lessons from the Los Angeles County Community
Disaster Resilience Project. Disaster Med Public Health Prep. 2015;9(5):484-488.
9. California Hospital Association. What is the difference between a tabletop
exercise, a drill, a functional exercise, and a full-scale exercise? Available at
http://www.calhospitalprepare.org/post/what-difference-between-tabletop-exercise-drill-functional-exercise-and-full-scale-exercise. Accessed February 4,
2016.
10. Lerner EB, Schwartz RB, Coule PL, Pirrallo RG. Use of SALT Triage in a
simulated mass-casualty incident. Prehosp Emerg Care. 2009;14(1):21-25.
11. Gnauck KA, Nufer KE, LaValley JM, et al. Do pediatric and adult disaster
victims differ? A descriptive analysis of clinical encounters from four natural
disaster DMAT deployments. Prehosp Disast Med. 2007;22(1):67-73.
12. Weiner DL, Manzi SF, Waltzman ML, et al. FEMA's organized response with a
pediatric subspecialty team: the National Disaster Medical System response: a
pediatric perspective. Pediatrics. 2006;117(5 Pt 3):S405-S411.
13. The Pediatric Disaster Preparedness Subcommittee (California). EMSC Pediatric
Disaster Preparedness Guidelines: LEMSAS.
http://www.emsa.ca.gov/media/default/pdf/emsa197.pdf. Accessed January 28,
2016.
14. Baker MD. Antidotes for nerve agent poisoning: should we differentiate children
from adults? Curr Opin Pediatr. 2007;19(2):211-215.
15. Quail MT, Shannon MW. Pralidoxime safety and toxicity in children. Prehosp Emerg Care. 2007;11(1):36-41.
16. Brown JC, Tuuri RE, Akhter S, et al. Lacerations and embedded needles caused
by epinephrine autoinjector use in children. Ann Emerg Med. 2015 Oct 3. pii:
S0196-0644(15)00588-0. doi:10.1016/j.annemergmed.2015.07.011. [Epub ahead
of print]
17. Mancini AJ. Skin. Pediatrics. 2004;113(4 suppl):1114-1119.
18. Perry JN, Hooper VD, Masiongale J. Reduction of preoperative anxiety in
pediatric surgery patients using age-appropriate teaching interventions. J
Perianesth Nurs. 2012;27(2):69-81.
19. Schonfeld DJ, Gurwitch RH. Addressing disaster mental health needs of children:
practical guidance for pediatric emergency health care providers. Clin Ped Emerg
Med. 2009;10(3):208-215.
20. Cornell University Cooperative Extension. Natural and weather-related disasters.
Available at
http://emergencypreparedness.cce.cornell.edu/disasters/Pages/default.aspx.
Accessed February 2, 2016.
21. Campbell CM, Baker MD, Monroe KW. Prevention of child injuries during
tornadoes: cases from the 2011 tornado outbreak in Alabama. Pediatr Emerg
Care. 2012;28(12):1389-1390.
22. Centers for Disease Control and Prevention (CDC). Heat-related deaths—United
States, 1999-2003. MMWR Morb Mortal Wkly Rep. 2006;55(29):796-798.
23. World Health Organization. Flooding and communicable diseases fact sheet.
Available at http://www.who.int/hac/techguidance/ems/flood_cds/en/. Accessed
February 5, 2016.
24. State of Connecticut Department of Public Health. Hurricanes: Important health
information. Available at
http://www.ct.gov/dph/cwp/view.asp?a=3115&q=513014. Accessed February 1,
2016.
25. World Health Organization. FAQs: Japan tsunami concerns. March 2011.
Available at http://www.who.int/hac/crises/jpn/faqs_tsunami/en/. Accessed
February 4, 2016.
26. US Geological Service Volcanic Ash Impacts Working Group. Volcanic ash
impacts & mitigation: Health. Available at
https://volcanoes.usgs.gov/volcanic_ash/health.html. Accessed February 4, 2016.
27. Finlay SE, Moffat A, Gazzard R, et al. Health impacts of wildfires. PLoS Curr. 2012 Nov 2;4:e4f959951cce2c.
28. Weir E. Tornadoes and disaster management. CMAJ. 2000;163(6):756.
29. Jhung MA, Shehab N, Rohr-Allegrini C, et al. Chronic disease and disasters
medication demands of Hurricane Katrina evacuees. Am J Prev Med. 2007;33(3):207-10.
30. Centers for Disease Control and Prevention. Bioterrorism overview. Available at
http://emergency.cdc.gov/bioterrorism/overview.asp. Accessed February 5, 2016.
31. United States Army Medical research Institute of Infectious Disease. Medical
management of biological casualties handbook. 7th edition. Available at
http://www.usamriid.army.mil/education/bluebookpdf/USAMRIID%20BlueBook
%207th%20Edition%20-%20Sep%202011.pdf. Accessed February 5, 2016.
32. Ganesan K, Raza SK, Vijayaraghavan R. Chemical warfarin agents. J Pharm
Bioallied Sci. 2010; 2(3):166-179.
33. Chemical-biological terrorism and its impact of children. Pediatrics. 2006;118(3):1267-1278.
34. Lansdowne K, Scully CG, Galeotti L, et al. Recent advances in medical device
triage technologies for chemical, biological, radiological, and nuclear events. Prehosp Disaster Med. 2015;30(3):320-323.
35. Ramesh AC, Kumar S. Triage, monitoring, and treatment of mass casualty events
involving chemical, biological, radiological, or nuclear agents. J Pharm Bioallied
Sci. 2010;2(3):239-247.
36. National Security Staff Interagency Policy Coordination Subcommittee for
Preparedness and Response to Radiological and Nuclear Threats. Planning
guidance for response to nuclear detonation, 2010. Available at
http://www.epa.gov/radiation/docs/er/planning-guidance-for-response-to-nuclear-detonation-2-edition-final.pdf. Accessed January 31, 2016.
37. World Nuclear Association. Fukushima accident. January 2016. Available at
http://www.world-nuclear.org/information-library/safety-and-security/safety-of-plants/fukushima-accident.aspx. Accessed February 5, 2016.
38. Marx J, Hockberger R, Walls R, Adams J, Rosen P. Rosen's Emergency
Medicine - Concepts and Clinical Practice. 7th ed. Philadelphia, Pennsylvania:
Mosby/Elsevier; 2010.
39. AAP Health Initiatives. Children and Disasters. Radiologic or nuclear terrorism
and agents. Available at https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Children-and-Disasters/Pages/Radiologic-or-Nuclear-Terrorism-and-Agents.aspx. Accessed February 5, 2016.
40. US Department of Health and Human Services. White cell growth
factors/cytokines-radiation emergency medical management. REMM Web site.
Available at http://www.remm.nlm.gov/cytokines.htm. Accessed January 31,
2016.
41. Radiation and Emergency Medical Management. Triage category and cytokine
(G-CSF) use after a nuclear detonation. Available at
http://www.remm.nlm.gov/triagetool5.htm. Accessed February 5, 2016.
42. U.S. Environmental Protection Agency. Protective action guides and planning
guidance for radiological incidents. March 2013.
43. Revkin AC. Nuclear risk and fear, from Hiroshima to Fukushima. New York
Times. March 10, 2012. Available at
http://dotearth.blogs.nytimes.com/2012/03/10/nuclear-risk-and-fear-from-hiroshima-to-fukushima/?_r=0. Accessed February 5, 2016.
44. Yamashita S, Takamura N. Post-crisis efforts towards recovery and resilience
after the Fukushima Daiichi Nuclear Power Plant accident. Jpn J Clin Oncol. 2015;45(8):700-7.
45. American Society of Health-System Pharmacists. ASHP statement on the role of
health-system pharmacists in emergency preparedness. Am J Health-Syst Pharm.
2003;60:1993-1995.
46. American Society of Health-System Pharmacists. ASHP statement on pharmacy services to the emergency department. Am J Health-Syst Pharm. 2008; 65: 2380-2383.
Back to Top