
Expired activity
Please go to the PowerPak
homepage and select a course.
Squashing the Common Head Lice Myths: Update on Eradication and Resistance Patterns
CURRENT STATUS OF HEAD LICE MANAGEMENT
The head louse, Pediculus humanus capitis, is a parasitic insect that inhabits the head, eyebrows, and eyelashes of humans only.1 While it does not pose a serious health threat, pediculosis is an extraordinarily frustrating, poorly understood, and often mismanaged public health problem. The challenges associated with detecting and eradicating head lice affect parents and families, organizations such as schools and summer camps, doctors' offices, and employers.2 Health care providers require current, accurate information about risk factors for head lice risk infestation or eradication methods.3 The emergence of pesticide-resistant strains of the louseis a significant driver of continued lice outbreaks and treatment failures.4,5 However, health care professionals including physicians, nurses, and pharmacists may be unaware of local resistance patterns and how these patterns influence the effectiveness of treatment recommendations. This review discusses the most recently available resistance data in the context of multidisciplinary head lice management, in order to provide communities with accurate, "myth-free" information about these infestations.
Cost and Impact of Head Lice Epidemic
With an incidence rate ranging from 6 to 12 million infestations in the U.S. each year, one might say that the country is crawling with head lice.1 Overall U.S. prevalence rates tend to be low compared with areas where grooming and sanitation practices are less stringent.6 The lice epidemic has tangible effects well beyond mere annoyance and embarrassment—in fact, it is responsible for a significant economic burden in terms of both direct treatment costs and indirect costs associated with missed work and school time.7 Total direct plus indirect costs have been reported at ranges from $367 million to as high $1 billion per year.5,8 An increasing incidence of infestations among the primary age group affected—children aged 3 to 12—is likely to continue to escalate these costs.8 Direct costs are also escalated by treatment failures, which may result in repeated attempts with a single treatment or use of multiple treatments. Some studies suggest that patients or families self-treat lice infestations an average of 5 times before they seek advice from a health care professional.9 This increases the expense of products purchased in failed attempts to eradicate the infestation. Expensive nit-combing services are popular in many areas and can cost $150 or more per treatment.10 Indirect costs reflect lost school and workdays, including days when a parent is unable to attend work because a child is excluded from the classroom. One source suggests that lost wages may average $2,720 per family with each infestation.2
How Pediculosis is Currently Managed
Management of head lice often goes amiss because of misconceptions about how the lice are contracted and spread and how to best eradicate the outbreak. Schools, summer camps, and institutions still cling to outdated "no nit" policies.7,11 The American Academy of Pediatrics (AAP) has spoken out against "no nit" policies and the exclusion of affected children from activities, yet such policies remain in place in many areas.12 Misunderstandings about how to kill the lice lead to inconsistent recommendations about the best ways to manage a lice infestation—a pediatrician may suggest that patients ask a pharmacist for an over-the-counter pediculicide; a pharmacist may suggest the patient seek medical advice to obtain a prescription agent; teachers, school nurses, coaches, and others in the community may recommend nit-combing and barrier methods (such as topical oils) only and discourage families from using pediculicides, especially for young children. Knowledge about the safety and effectiveness of currently available treatments for head lice and the correct manner of their application can help health care professionals to guide patients toward a quicker eradication of this condition.
MANAGING HEAD LICE WITH PEDICULICIDAL AGENTS
Pediculicides available in the U.S. include both over-the-counter (OTC) and prescription-only agents (Table 1).13 Some agents have a residual effect that allows them to kill both the louse and viable eggs. Others kill the louse only, which entails the need for combing and may require reapplication to kill any newly hatched eggs. Despite reported resistance to these agents, the AAP and Centers for Disease Control and Prevention (CDC) guideline statements recommend permethrin- or pyrethrin-based pediculicides as first-line agents.12,13
| Table 1. U.S. Food and Drug Administration-Approved Treatments for Head Lice |
| Agent/Brands |
Indications |
Administration |
Notes |
|
Permethrin 1%14
Nix
|
OTC; Indicated for adults and children aged ≥ 2 months.
(Permethrin cream 5%, Rx only, is indicated for scabies.)
|
Wash hair with regular shampoo. Apply product to damp hair on leave for 10 minutes.
|
Label recommends retreatment after 7 days if live lice are observed. Prone to resistance.
Pregnancy category B
|
|
Pyrethrin 4%15
RID
|
OTC; Indicated for adults and children age ≥ 2 years.
|
Leave on dry hair for 10 minutes and rinse out. Retreat after 7–10 days to kill newly hatched lice.
|
Kills live lice but not eggs. Retreatment is recommended.
Pregnancy category B
|
|
Spinosad 0.9%16
Natroba
|
Rx only. Indicated for adults and for children ≥ 6 months of age.
|
Topical suspension; apply to dry hair and scalp and rinse off after 10 minutes.
|
Kills both lice and eggs, which eliminates need for nit combing.
Pregnancy category B
|
|
Benzyl alcohol 5%17
Ulesfia
|
Rx only. Indicated for adults and children ≥ 6 months of age.
|
Lotion in 3 dosage strengths; application depends upon length of hair.
|
Agent works via smothering. No ovicidal activity, so eggs/nits must be removed.
Pregnancy category B
|
|
Ivermectin 0.5%18
Sklice
|
Rx only. Indicated for adults and children ≥ 6 months of age.
|
Lotion; apply to dry hair and scalp and rinse off after 10 minutes.
|
Does not require nit combing.
Pregnancy category C
|
|
Lindane 1%19
Kwell Shampoo
|
Rx only. Indicated only for patients who cannot tolerate or have failed first-line treatment with safer medications for treatment of lice. Observe contraindications.
|
Dose: 1 ounce; patients with longer hair may require 2 ounces. Apply to dry hair without adding water. Keep in place for 4 minutes, then lather and rinse immediately. Avoid unnecessary contact of lather with other body surfaces. Do not retreat.
|
Associated with serious safety concerns, including black box warning on risks of neurotoxicity. Banned in State of California.
Do not prescribe more than 2 ounces for larger adults.
Pregnancy category C
|
|
Malathion 0.5%20
Ovide
|
Rx only. Safety in children under 6 years of age has not been established.
|
Topical lotion; leave uncovered on dry hair for 10–12 hours, rinse off. Retreat in 7–9 days if lice are still present.
|
Early-life exposure to organophosphates has been associated with behavioral and developmental disorders.
Pregnancy category B
|
Pediculicide safety is a particular concern, especially for parents of young children.21 Many parents avoid using a pediculicide to kill head lice because of toxicity concerns, and may instead opt for combing or use unproven remedies that involve applying oily substances to the scalp in an effort to "smother" the live lice. (A common folk remedy involves covering the head with mayonnaise and a shower cap.) Improved patient education about safety and toxicity of various pediculicides is needed.22
Permethrin and Pyrethrin
The permethrin- and pyrethrin-based agents are not associated with known toxicities in humans. Pyrethrins are extracted from the flower of the pyrethrum plant, Chrysanthemum cinerariaefolium.23 Pyrethrins do not have a residual pediculicidal effect, so re-treatment is necessary 7 to 10 days later to kill newly hatched lice. The synthetic form, permethrin, is more potent and has some residual pediculicidal effects, but the labeling recommends retreatment after 7 days if live lice are observed.24
Spinosad
Spinosad is among the newer prescription-only pediculicides.25 Spinosad is derived by fermentation of the soil bacterium Saccharopolyspora spinosa. Spinosad kills insects through hyperexcitation of the nervous system and other neurotransmitter effects, but is not associated with cross-resistance with other insecticides.26 Preclinical studies show that spinosad is not acutely toxic to mammals and is nonhazardous by oral, dermal, or other routes. In long-term studies in animals, spinosad was not associated with adverse safety signals or teratogenicity.27
Ivermectin
Ivermectin is a broad-spectrum antiparasitic indicated for both human and veterinary applications.18 It is active against a number of parasite types including scabies, head lice, and bed bugs in humans and heartworm in animals. This agent paralyzes and kills lice by increasing the permeability of the parasite's cell membranes.28 Oral ivermectin is indicated for treatment of parasitic infections caused by Onchocerca volvulus and Strongyloides stercoralis but is not indicated for the treatment of head lice.18, 24
Lindane
Because of serious safety concerns, lindane is used only rarely for eradication of lice. This agent is not recommended by AAP because of a black box warning relating to the risk of serious neurotoxicity.29 The labeling restricts use to individuals who 1) cannot tolerate other approved therapies or 2) have failed treatment with other approved therapies. The black box warning emphasizes that lindane should not be used on premature infants and individuals with known uncontrolled seizure disorders, and should be used with caution in infants, children, the elderly, and individuals with a skin condition such as psoriasis or dermatitis. A person weighing less than 110 pounds (50 kg) may be at risk for serious neurotoxicity with the use of lindane.19 Seizures and deaths due to neurotoxicity have occurred even with a single lindane application.19
Malathion
Malathion is an insecticide in the chemical family of organophosphates.20 Malathion is not recommended for children under the age of 6 years. Studies have linked early childhood exposure to organophosphate insecticides with reductions in IQ and attention-deficit/hyperactivity disorder.30 The most recent AAP Committee on Infectious Diseases guideline on head lice lists this agent as "not recommended."12 Malathion must be left on for 8 to 12 hours, but this substance is flammable so users must be warned to avoid contact with electrical heat sources such as hair dryers and curling irons as well as sources of flame such as cigarettes.20
Another safety concern is whether pediculicide exposure is safe for pregnant women or those who are planning a pregnancy. While there are limited data on the teratogenic potential of available pediculicides, guidance from the U.S. Food and Drug Administration (FDA) to industry for developing topical agents for head lice treatment recommends that the teratogenicity of the active ingredients should be evaluated.31
IMPACT OF PERMETHRIN/PYRETHRIN RESISTANCE ON HEAD LICE TREATMENT
Permethrin and pyrethrin kill lice via a common mechanism, by binding to a site in the louse nervous system that causes nerve paralysis and death.32 In recent years, resistant louse strains have developed a heritable insensitivity at the target site in the nervous system, known as knockdown resistance (kdr).33 In the United Kingdom, permethrin has been regarded as "virtually useless" since 1999, due to resistance problems.34 In 2014 a comprehensive examination of head louse samples from across the U.S. and Canada by Yoon and colleagues showed the frequency of the permethrin-resistant "TI" genotype mutation at 99.6% of U.S. areas sampled and 97.1% of those in Canada (Figure 1).33
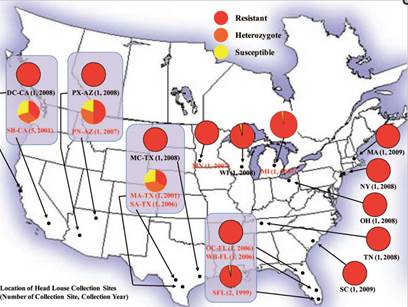 |
| Figure 1. Red circles indicate areas where lice samples were tested and found resistant to pyrethrins/pyrethroids. Source: Yoon KS, et al. Knockdown resistance allele frequencies in North American head louse (Anoplura: Pediculidae) populations. J Med Entomol. 2014;51(2):450-457. |
These authors speculated that high "selection pressure" and repeated use of pyrethrins/pyrethroids are main causes of the spike in resistance patterns observed between 1999 and 2009.33 Studies of these pediculicides conducted in the late 1980s to mid-1990s showed effectiveness rates of 96% to 100%, but efficacy began to drop soon afterward.23,35
To determine the current status of resistance to pyrethrin and pyrethroid insecticides in the U.S., Gellatly and colleagues collected 14,281 louse samples from 138 collection sites (479 human subjects) across 48 states between July 2013 and May 2015.4 A total of 1,925 lice were analyzed using quantitative sequencing. The researchers looked for 3 different kdr-type mutations and averaged the percentage of resistant alleles found, reporting the mean resistance allele frequency (% RAF) across the samples. The overall mean % RAF (± SD) for all analyzed lice was 98.3% (± 10%). More than 95% of the collection sites (132 of 138) had a mean % RAF of 100%, 5 sites (3.7%) had intermediate values, and only 1 site had no mutations found. Forty-two states (88%) had a mean % RAF of 100% (Figure 2).4
 |
| Figure 2. Mean % RAF values from head lice collected in the United States between 2013 and 2015. Red dot = fully resistant (RAF = 100%); orange stars (50% ≤ RAF < 99%) for intermediate resistance are marked in 5 states. Fully susceptible (green star) was found in only 1 state (sample taken from Frankenmuth, Michigan). No samples were taken from Alaska or West Virginia. Reprinted under Creative Commons Attribution license 4.0 from Gellatly et al. J Med Entomol. 2016. |
This study also correlated kdr-type mutations with loss of efficacy of an OTC permethrin formulation. The authors stated, "These data provide a plausible reason for the decrease in the effectiveness of permethrin...which is the parallel increase of kdr-type mutations in lice over time."4
While resistance rates in head lice have been reported in the U.S. over a period of several decades, the implications of resistance may be unclear to health professionals, who base treatment recommendations on past experience rather than knowledge of resistance patterns.36 Guideline recommendations by the AAP and others recommend observing local resistance rates. The most recent AAP head lice position paper updated in April 2015 states, "Unless resistance has been seen in the community, pediatricians and parents should consider using over-the-counter medications containing 1% permethrin or pyrethrins as a first choice of treatment for active lice infestations."12 However, the report fails to explain how a health professional can determine local resistance data.
A few studies have compared the efficacy of permethrin and pyrethrin treatment with that of other pediculicides. For example, a regimen of spinosad without nit coming was compared with permethrin plus nit combing in 2 Phase III multicenter studies encompassing a total of 1,038 subjects with head lice or household exposure to head lice.27 At the end of a 21-day evaluation period, between 84.6% and 86.7% of spinosad-treated patients were lice-free (2 studies reported), compared with 44.9% and 42.9% of permethrin-treated subjects (P < 0.001). Adverse events were mild to moderate and similar across treatment groups, including eye irritation (permethrin), eye redness, and application-site irritation (both medications). Most spinosad-treated participants required only 1 application while most of the permethrin-treated subjects required 2 applications.27
Ivermectin has been compared head-to-head with malathion, but only in its oral formulation. Under laboratory conditions, topical ivermectin has been shown to be active against permethrin-resistant head lice.37 Because ivermectin kills lice via a different mechanism, this suggests that the topical form of ivermectin may be a treatment option in cases of treatment failure with permethrin or pyrethrins.38
IMPACT OF MYTHS AND MISCONCEPTIONS ON HEAD LICE MANAGEMENT
Misunderstandings and misinformation about ineffective therapies for head lice tend to spread as rampantly as the lice themselves.39 Internet sites geared toward desperate parents often tout "fail-safe" schemes or folk remedies that describe laborious steps for cleaning the house, isolating a child's bedding and toys, and having the child sleep with a headful of mayonnaise or olive oil. Some people still resort to dangerous practices such as using kerosene or gasoline on the hair.40
Mistreatment of head lice falls into the category of both over-treatment and under-treatment. If a recommended treatment is not effective, the user is often blamed for nonadherence or incorrect application.40 Conversely, when treatment is ineffective due to incorrect administration, this is sometimes mistaken for drug resistance.5 To get a better handle on head lice management, providers at all levels need updated and accurate knowledge and an awareness of how this problem impacts families, especially those with young children who are in the highest risk groups.
Diagnosis: When is a Nit Not a Nit?
Although the diagnosis may seem obvious, head lice are often misdiagnosed or overdiagnosed, especially if one is basing a diagnosis solely on the presence of nits (empty egg casings).7,41 In the absence of a live louse, small particles in the hair are often mistaken for an infestation. For patients who have been exposed to lice, nits are commonly mistaken for viable eggs and result in overtreatment.
There is evidence that consumers and health care personnel—even school nurses—incorrectly identify artifacts in the hair, including dandruff or skin flakes or hair product debris, as often as they correctly identify a louse or nit.41 The most recent AAP Clinical Report on head lice management5 recommends that pediatricians and school nurses improve their skills in the identification of an active infestation with head lice to avoid treating patients unnecessarily or falsely identifying resistance in the community.12 Understanding the louse life cycle can help to identify the different stages of infestation (Table 2).42
|
Table 2. Life Cycle of a Head Louse42
Reproduction
- Adult female louse lives 3 to 4 weeks, can lay up to 10 eggs per day
- Eggs are attached to the hair shaft within 4mm of the scalp
- In about 7 to 12 days eggs hatch into nymphs
- Empty egg casings (which appear white on the hair shaft) are referred to as "nits" (some definitions of nit encompass both the viable eggs and the empty casings)
- Nymphs mature to adults after about 9 to 12 days
- Female lice mate and lay eggs within a few days of reaching adulthood

Source: Centers for Disease Control.1
Mealtimes
- The louse feeds on the host's blood every few hours
- Itching sensations may be caused by the parasite's saliva
- Head lice do not survive for more than a day or so away from the scalp
- Eggs are highly unlikely to hatch when removed from the scalp
|
Misconceptions and myths about lice, their life cycle, and how to eradicate an outbreak tend to spread even more quickly than the lice themselves. A summary of myths and facts on head lice is included in Table 3.1,5,41
| Table 3. Head Lice Myths and Facts1,5,41 |
| Myth |
Fact |
| Lice are easily spread between individuals, such as in a classroom or on a sports team. |
Head lice crawl but cannot fly or hop, so direct contact between heads is needed (e.g., 2 children sleeping in the same bed or sitting next to each other in a car). |
| Nits can be transferred from one head to another. |
Nits do not move after being laid, but remain stuck to the hair shaft. The most viable nits are those that are ≤6 mm from the scalp. Even viable nits do not transmit lice. Eggs cannot be transmitted from one head to another, nor can they fall off the hair shaft. Even if hair with a viable nit were to fall off, it will not hatch at temperatures lower than the human head. |
| Presence of a single nit is indicative of an active lice infestation. |
Presence of a live louse is the gold standard for an active infestation, not the mere presence of a nit. |
| Classroom checks and letters home help to limit spread of lice in schools. |
Letters from a school about an infestation may be a violation of privacy. There is no evidence that these policies reduce the spread of head lice. |
| Examination by a teacher or nurse is a good way to detect nits and louse infestation. |
Parents and teachers are usually unable to tell the difference between a nit and other debris in the hair. |
| Prophylactic treatment is a good idea if a case of head lice is detected in a child's classmate. |
Prophylactically treating others who were in contact with the person infected constitutes over-treatment. |
| No-nit policies are endorsed by the AAP and the CDC. |
Groups calling for elimination of no-nit policies include the AAP, CDC, and National Association of School Nurses |
| Head lice are not only unpleasant but may spread diseases. |
Head lice do not carry disease. |
| For head lice infestations in the home, fumigating the house and cleaning of all bedding, clothing, and stuffed toys is necessary. |
The CDC recommends vacuuming the floor and furniture where the infested person may have come in contact. Machine washing and drying clothing and bed linens is also recommended. However, it adds: "Spending much time and money on housecleaning activities is not necessary...do not use fumigant sprays, which can be toxic if inhaled or absorbed." |
| An active case of lice can be spread by dogs or cats. |
Head lice cannot spread to pets. |
| AAP=American Academy of Pediatrics; CDC=Centers for Disease Control and Prevention |
Persistence of "No-Nit" Policies in Schools and Institutions
Even though the AAP, CDC, and other organizations have advised against "no nit" policies for schools, summer camps, and other institutions, these policies continue to be in place. This means that if a child has a reported case of head lice, he or she cannot return to school (or must be sent home from camp) until no nits can be detected. Unfortunately, this may serve to redirect attention from undetected cases and focus unnecessary "punishment" on the person who has already under treatment. School children infected with lice lose an average of 4 days of school per year in areas where "no-nit" policies are enforced.12 There is no medical need to eliminate empty egg cases.12
Role of Physicians, Nurses, and Pharmacists in Patient Education About Head Lice
Pediatricians and other physicians may refer patients to the pharmacy shelf or a do-it-yourself method. However, it is important for physicians to guide parents accurately in head lice management to ensure safe and effective application of approved agents, and to avoid ineffective and possibly unsafe home remedies. For many patients, an application of an effective pediculicide as directed, and appropriate follow-up to confirm the eradication, can prevent many frustrating and failed attempts if the patient/parent attempts at self-treatment. An agent that does not require nit combing can help to improve adherence and provide added convenience for the family.25,37
Nurses, including school nurses and pediatric or family practice-based nurses, are an essential source for accurate patient/family education about head lice.11,39 It is important for the nurse to be able to instruct the patient correctly in the application of the particular agent recommended, as there is a large degree of variation among products. Finally, it is essential for nurses (especially school nurses) to be aware of methods for sensitively and discreetly addressing the issue of head lice.39
Pharmacists are often on the front lines when it comes to the war on head lice. Many parents and other affected individuals will seek help directly from a pharmacist for this problem. For a pharmacist in community-based practice, having accurate, up-to-date information about head lice treatment is essential. Patients frequently ask pharmacists for help choosing an appropriate agent, so familiarity with all OTC and prescription-only options is important. Pharmacists should ask consumers what methods they have previously tried, and whether they have received any treatment recommendations from physicians or nurses. With the introduction of more agents that are available by prescription, pharmacists need to be able to direct patients to their physicians when appropriate. When filling a pediculicide prescription or recommending an OTC agent, it is essential for pharmacists to be aware of the correct application of these agents and other steps involved in head lice eradication.3
CONCLUSION
Treatment of head lice should be a straightforward matter, but unfortunately these infestations are increasingly difficult to control. A significant factor is the widespread resistance of lice in the U.S. and elsewhere to the older pediculicides, especially permethrin and pyrethrin. Awareness of resistance patterns can help health care providers select appropriate treatments. In addition, awareness of the safety data and safe application of pediculicides is important to minimize toxicity and ensure correct use, especially in young children. Prevailing myths and misconceptions prevent effective head lice treatments from being applied promptly and correctly. When educating patients, parents, school officials, and others, it is essential that credible sources of information and current guidelines are used, rather than relying on outdated or inaccurate policies and practices.
References
- Centers for Disease Control and Prevention. Parasites - Lice - head lice. Frequently Asked Questions. Available at: http://www.cdc.gov/parasites/lice/head/gen_info/faqs.html.
- Hansen RC, O'Haver J. Economic considerations associated with Pediculus humanus capitis infestation. Clin Pediatr (Phila). 2004;43(6):523-527.
- Olowokure B, Jenkinson H, Beaumont M, et al. The knowledge of healthcare professionals with regard to the treatment and prevention of head lice. Int J Environ Health Res. 2003;13(1):11-15.
- Gellatly KJ, Krim S, Palenchar DJ, et al. Expansion of the knockdown resistance frequency map for human head lice (Phthiraptera: Pediculidae) in the United States using quantitative sequencing. J Med Entomol. 2016.
- Frankowski BL, Bocchini JA, Jr. Head lice. Pediatrics. 2010;126(2):392-403.
- Feldmeier H. Pediculosis capitis: new insights into epidemiology, diagnosis and treatment. Eur J Clin Microbiol Infect Dis. 2012;31(9):2105-2110.
- Mumcuoglu KY, Meinking TA, Burkhart CN, et al. Head louse infestations: the "no nit" policy and its consequences. Int J Dermatol. 2006;45(8):891-896.
- Hansen RC. Overview: the state of head lice management and control. Am J Manag Care. 2004;10(9 Suppl):S260-263.
- West DP. Head lice treatment costs and the impact on managed care. Am J Manag Care. 2004;10(9 Suppl):S277-282.
- A lousy choice: When kids get lice, should parents DIY or go pro? Dec 10, 2013, TODAY Parents. Available at: http://www.today.com/parents/lousy-choice-when-kids-get-lice-should-parents-diy-or-2D11709198.
- Rollins JA. Back to school? The 'no nit' policy. Pediatr Nurs. 2010;36(5):236-237.
- Devore CD, Schutze GE. AAP Council on School Health, Committee on Infectious Diseases. Head lice. Pediatrics. 2015;135(5):e1355–e1365.
- Centers for Disease Control and Prevention. Parasites - Lice - head lice. Treatment. Updated Dec 28, 2015. Available at: http://www.cdc.gov/parasites/lice/head/treatment.html.
- Nix [package insert]. Insight Pharmaceuticals; 2009.
- Rid [package insert]. Morristown, NJ: Bayer; 2015.
- Natroba (spinosad) [package insert]. Carmel, IN: ParaPRO; 2014.
- Ulesfia (benzyl alcohol) [package insert]. Dublin, Ireland: Lachlan Pharmaceuticals; 2015.
- Sklice (ivermectin) lotion [package insert]. Swiftwater, PA: Sanofi Pasteur; 2012.
- Food and Drug Administration. Lindane Shampoo revised labeling. Updated 7/16/2015. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm110452.htm.
- Ovide (malathion) lotion [package insert]. Lakewood, NJ: Medicis.
- Burkhart CG, Burkhart CN. Safety and efficacy of pediculicides for head lice. Expert Opin Drug Saf. 2006;5(1):169-179.
- Andresen K, McCarthy AM. A policy change strategy for head lice management. J Sch Nurs. 2009;25(6):407-416.
- Bainbridge CV, Klein GL, Neibart SI, et al. Comparative study of the clinical effectiveness of a pyrethrin-based pediculicide with combing versus a permethrin-based pediculicide with combing. Clin Pediatr. 1998;37:17-22.
- Mazurek CM, Lee NP. How to manage head lice. West J Med. 2000;172(5):342-345.
- Aditya S, Rattan A. Spinosad: An effective and safe pediculicide. Indian Dermatol Online J. 2012;3(3):213-214.
- Villegas SC. Spinosad for the treatment of head lice infestations. Drugs Today (Barc). 2012;48(9):595-599.
- Stough D, Shellabarger S, Quiring J, et al. Efficacy and safety of spinosad and permethrin creme rinses for pediculosis capitis (head lice). Pediatrics. 2009;124(3):e389-395.
- Strycharz JP, Berge NM, Alves AM, et al. Ivermectin acts as a posteclosion nymphicide by reducing blood feeding of human head lice (Anoplura: Pediculidae) that hatched from treated eggs. J Med Entomol. 2011;48(6):1174-1182.
- Wiles DA, Russell JL, Olson KR, et al. Massive lindane overdose with toxicokinetics analysis. J Med Toxicol. 2015;11(1):106-109.
- Roberts JR, Karr CJ. Pesticide exposure in children. Pediatrics. 2012;130(6):e1765-1788.
- Food and Drug Administration. Head Lice Infestation: Developing drugs for topical treatment, guidance for industry. Dec 2015. Available at: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM476999.pdf.
- Clark JM. Determination, mechanism and monitoring of knockdown resistance in permethrin-resistant human head lice, Pediculus humanus capitis. J Asia-Pacific Entomol. 2009;12(1):1-7.
- Yoon KS, Previte DJ, Hodgdon HE, et al. Knockdown resistance allele frequencies in North American head louse (Anoplura: Pediculidae) populations. J Med Entomol. 2014;51(2):450-457.
- Dawes M, Hicks NR, Fleminger M, et al. Evidence based case report: treatment for head lice. Bmj. 1999;318(7180):385-386.
- Taplin D, Meinking TL, Castillero PM, et al. Permethrin 1% creme rinse for the treatment of Pediculus humanus var capitis infestation. Pediatr Dermatol. 1986;3:344-348.
- Yoon KS, Gao JR, Lee SH, et al. Permethrin-resistant human head lice, Pediculus capitis, and their treatment. Arch Dermatol. 2003;139(8):994-1000.
- Pariser DM, Meinking TL, Bell M, et al. Topical 0.5% ivermectin lotion for treatment of head lice. N Engl J Med. 2012;367(18):1687-1693.
- Deeks LS, Naunton M, Currie MJ, et al. Topical ivermectin 0.5% lotion for treatment of head lice. Ann Pharmacother. 2013;47(9):1161-1167.
- Pontius DJ. Demystifying pediculosis: school nurses taking the lead. Pediatr Nurs. 2014;40(5):226-235.
- Pray WS. Pediculocide resistance in head lice: a survey. Hosp Pharm. 2003;38(3):241-246.
- Pollack RJ, Kiszewski AE, Spielman A. Overdiagnosis and consequent mismanagement of head louse infestations in North America. Ped Infect Dis J. 2000;19(8):689-693; discussion 694.
- Centers for Disease Control. Parasites - Lice - Head Lice. Biology. Updated Sept 2, 2015. Available at: http://www.cdc.gov/parasites/lice/head/biology.html.
Back to Top