
Expired activity
Please go to the PowerPak
homepage and select a course.
2017 Update: Module 1. Introduction to Medication Therapy Management (MTM)
What is Medication Therapy Management (MTM)?
MTM usually refers to counseling services between a pharmacist (or nurse or other health professional) and a patient (or caregiver). In MTM, the patient's medications are evaluated to make sure they are:1
- prescribed appropriately
- safe and effective for that person
- being taken correctly, at the correct dose and times
- able to be taken by the patient as intended
- financially viable for the patient
MTM is being promoted to help address some of the major problems of healthcare delivery. These include:
- high costs of medications
- potential for medication errors
- poor adherence and inappropriate use of medications
Pharmacists are recognized as among the most appropriate sources for MTM services. However, support and participation from the technician are essential. In fact, many pharmacy educators believe that in order to carry out MTM efficiently, pharmacists need to work alongside technicians who are trained and able to take on many of the roles.
How Medicare Part D Has Influenced MTM
Medicare Part D was introduced as the first outpatient prescription drug benefit for patients who have Medicare coverage. Medicare is a government program that provides health insurance for Americans aged 65 and older, and for younger people with certain disabilities. Legislation known as the "Medicare Prescription Drug Improvement and Modernization Act" (MMA)2 requires that some Medicare Part D recipients who have chronic illnesses should receive MTM services to help contain costs and better manage the complex aspects of treating these conditions.3,4 The basic goals for Medicare Part D–sponsored MTM are outlined in Table 1.
| Table 1. Requirements of MTM Under Medicare Part D4 |
Medicare Part D sponsors are private insurers and others that contract to provide healthcare services to Medicare patients. Sponsors must offer MTM services that:
- Help qualified patients who receive drug benefits under Part D to optimize use of their medications;
- Reduce the risk of adverse events and drug interactions among these patients;
- Enhance cooperation between pharmacists and physicians.
|
| Centers for Medicare & Medicaid Services. 2017 Medicare Part D Medication Therapy Management (MTM) Programs. Fact Sheet: Summary of 2017 MTM Programs. August 16, 2017. Available at: https://www.cms.gov/Medicare/Prescription–Drug–
Coverage/PrescriptionDrugCovContra/Downloads/CY2017–MTM–Fact–Sheet.pdf4 |
Rising Drug Costs Drive the Need for MTM
For the Medicare program, cost savings is a major goal for MTM. Americans' spending on both prescription and nonprescription drugs has grown exponentially over the past 50 years, from $4 billion to over $324 billion (Figure 1).5 Expenditures for drugs are projected to grow an additional 6.7% per year through the year 2025.6
| Figure 1. Rise in U.S. Spending on Medications5 |
 |
| Sources: IMS Institute for Health Informatics; Centers for Medicare & Medicaid Services (CMS), National Health Expenditure (NHE) Fact Sheet.6 |
People aged 65 and older (those eligible for Medicare) are the highest consumers of prescription drugs. Medicare recipients who have multiple chronic illnesses:7
- see an average of 13 different physicians;
- account for 76% of all hospital admissions;
- are 100 times more likely to have a preventable hospitalization versus those with no chronic conditions.
Rising costs are also related to medication complications and errors.8–11 For example, in a period of just 5 years (1995 to 2000), the cost of drug–related complications in non–hospitalized patients rose from $76 billion to $177 billion.12 These costs are likely to continue to increase as a larger segment of the population reaches older ages. MTM services are aimed at reducing and preventing complications, and inappropriate use of medications that drive up costs.
Defining MTM
The Medicine Modernization Act of 2003 defines MTM as:2
- A program of drug therapy management that may be furnished by a pharmacist;
- Designed to ensure that covered Part D drugs under the prescription drug plan are appropriately used;
- Designed to optimize therapeutic outcomes through improved medication use and reduced risk of adverse drug events.
A group of 11 pharmacy organizations gathered in 2004 to better define MTM. The group determined that a program that provides MTM services should include:13
- Individualized services provided directly by a pharmacist to the patient;
- Face–to–face interaction between the patient and the pharmacist;
- Opportunities for pharmacists to identify patients who should receive MTM services;
- Payment for MTM services based on the time and resources involved.
Where Do Pharmacy Technicians Fit In?
MTM services are well suited for a pharmacist's skill set and training, and this is where pharmacy technicians come in. A trend is occurring now in which technicians are taking on many of the traditional roles of pharmacists, while pharmacists expand their roles in patient counseling and medical decision making (Figure 2). Pharmacy technicians are pursuing advanced training and many are receiving certification from the Pharmacy Technician Certification Board (PTCB) to take full advantage of their training.
How does this apply to MTM? Technicians' skill sets are well suited to many of the essential steps involved in preparing for and executing MTM. Training in MTM can help to expand on these skills. These may include:
- Identifying patients who may be candidates for MTM services
- Collecting patient medical records, lab results, and other information needed for MTM
- Performing screening steps with patients (such as, to determine health literacy)
- Helping to develop the main MTM documents, such as the Personal Medication List (PML) and Therapeutic Action Plan
- Helping patients work out drug benefit questions and challenges
- Processing paperwork to receive reimbursement for MTM services
| Figure 2. Changes in Pharmacy Practice and the Role of the Technician |
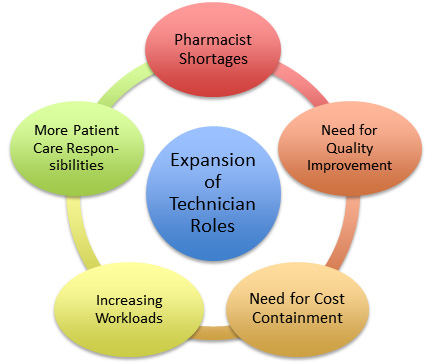 |
Changes in the laws in many states are expanding the responsibilities of pharmacists and the services for which they can receive payment. A U.S. Surgeon General's report states, "After an initial diagnosis is made, pharmacists deliver many patient care services—and function as healthcare providers—in a variety of practice settings through collaborative practice agreements, to manage disease (where medications are the primary mode of treatment)."14
In recent years more states (including California, North Dakota, Oregon, Tennessee, Washington, and Wisconsin) have authorized expanded roles for pharmacists as healthcare providers. Some of these expanded roles are tied to reimbursement. For example, in California passage of the legislation SB493 allows pharmacists to administer medications and immunizations, furnish hormonal contraception, and order and interpret tests, among other services.15 Federal legislation (the Pharmacy and Medically Underserved Areas Enhancement Act (HR 592/S314) has been proposed which would grant provider status for pharmacists through CMS and significantly expand reimbursement opportunities for pharmacists. This bill, an amendment to section 1861(s)(2) of the Social Security Act, would enable patients who are Medicare beneficiaries to access pharmacist–provided services under Medicare Part B. These services would be reimbursable under Medicare Part B if those patients reside in medically underserved communities and if the services are consistent with state scope of practice laws.16
Table 2 summarizes the roles of pharmacists listed in that document along with suggestions of how technicians can get involved to support those roles.
| Table 2. Expanding Roles of Pharmacists and Pharmacy Technicians |
| Pharmacist's Role |
Technician's Role |
| Perform patient assessments |
Document results of patient assessments |
| Initiate, adjust, or discontinue treatment to manage disease or manage medication use |
Assist in gathering background information (medical and pharmacy records) |
| Gather financial and demographic information |
Household size, finance status, insurance eligibility, need for copay assistance programs, etc. |
| Order, interpret, and monitor laboratory tests |
Place lab orders, obtain laboratory results; follow up with patients about recommended monitoring |
| Formulate clinical assessments and develop therapeutic plans |
Develop documents needed in MTM: Personal Medication List, Therapeutic Action Plan |
| Provide care coordination for wellness and prevention of disease |
Screen patients for health literacy |
| Develop partnerships with patients for ongoing (follow-up) care |
Assist patients with benefits and coverage and other troubleshooting |
| Adapted from 2011 U.S. Surgeon General Report on Pharmacist Utilization in Healthcare Delivery13 |
Overall Goals of MTM
A group of 11 pharmacy organizations—including the American Pharmacists Association (APhA) and the National Association of Chain Drug Stores Foundation—drafted an outline of basic steps for planning and delivering MTM. Many of these steps are also reflected in the CMS Medicare Part D guidelines for MTM.17 A summary of the main MTM steps is shown in Table 3.
| Table 3. Main Steps for MTM |
| MTM STEP |
EXAMPLES |
| 1. Gathering of patient information |
Medical records, drug history, lab results, insurance coverage |
| 2. Identifying issues and problems with the patient's medications |
Duplication of drugs, outdated prescriptions, discontinued medications, poor adherence due to side effects or lack of finances |
3. Determining an action plan for the
specific patient |
Streamlining therapies, switch to better-tolerated agents, helping patients get financial coverage. Examine barriers to adherence |
| 4. Documentation and follow-up |
Report back to physician, develop written plan for patient, update medical and pharmacy records, billing for MTM services, follow up with patients to encourage adherence to the plan. |
Questions and Answers About MTM
How is MTM different from other pharmacist services?
MTM differs from other patient counseling services provided by pharmacists in that it is patient–centered, rather than product–centered, as summarized in Table 4. With most pharmacy services, counseling happens when a patient brings in a prescription or refills a prescription, so the conversation focuses on education pertaining to the particular drug product. MTM takes a more comprehensive approach, focusing on the patient's disease state and complete healthcare. It examines what medications the patient is currently taking, as well as what treatments might have been overlooked.
| Table 4. Summary of MTM Goals |
Philosophy
- Patient–centered rather than product–centered
- Focuses on overall regimen rather than individual medication
- Collaboration among pharmacists and other healthcare providers
Outcomes
- Increase patients' understanding and self–management skills
- Improve patient adherence, thereby enhancing efficacy of medications
- Increase adherence to CMS quality performance standards
Mutual goals of MTM for pharmacy organizations, patients, and payers
- Reduce preventable adverse events and associated costs
- Reduce medication–related morbidity and mortality
- Reduce healthcare costs due to duplicate or unnecessary prescriptions
|
Does MTM work?
MTM and similar counseling services in the pharmacy can improve many aspects of healthcare, for patients and for the system overall. Research has shown benefits including:
- Increased access for certain patient groups that lack healthcare services
- Improved patient safety, by reducing errors in prescribing, dispensing, or taking medicines
- Support for physicians in the process of health education and counseling
- Enhanced cost–effectiveness
Studies have also demonstrated health benefits for patients with chronic diseases such as heart failure, diabetes, high blood pressure, and high cholesterol.18 These benefits have included better control of diabetes, more foot examinations for patients with diabetes, reduced blood pressure and cholesterol, and fewer adverse drug reactions.
In a 2011 study involving the Connecticut Medicaid system:19
- 369 patient–pharmacist encounters were analyzed
- 917 drug–therapy problems were identified by pharmacists
- 78% were resolved, without referring patient back to primary care provider
- 82% of prescribers made changes in therapy based on MTM recommendations
How are patients selected for MTM?
Almost anyone who has problems or questions about their medications can benefit from MTM—
including people who are not aware that a problem exists. However, the best targets for MTM services are usually patients who have chronic diseases and who are taking multiple medications. To get MTM services paid for through Medicare Part D, patients must meet 3 basic conditions:
- Have at least 2 "core chronic disease states" such as cardiovascular disease. These chronic diseases are listed in Module 6.
- Be taking multiple chronic or maintenance prescription medications
- Be likely to incur high annual drug costs.
Outside of Medicare Part D, any patient may receive MTM services at the request of their physician, through their employer, at the invitation of the pharmacist, or by self–referral. Transitions of care—such as when a patient is discharged from the hospital or switches physicians—are ideal times to review the medication history and address potential problems.
How can MTM services be adapted to fit our pharmacy practice?
MTM services can apply to virtually any patient, in any practice setting.20 The way MTM services are delivered is rapidly changing. MTM services may be provided in hospital settings, community and retail pharmacies, and as part of interdisciplinary teams of doctors, pharmacists, and other healthcare professionals (such as a patient–centered medical home). Table 5 lists questions that pharmacists, technicians, and others on the team may want to consider when planning for a new MTM service.
| Table 5. Questions to Consider When Planning an MTM Service |
- How will MTM services affect workload?
- Time, workflow challenges
- Administrative requirements
- Is there a need to create a space or find a space for face–to–face MTM consults?
- Space for in–person MTM consults
- Are phone or video consults viable?
- What patient populations will be targeted?
- How will patients be recruited?
- How will issues such as language/cultural barriers be addressed?
- What methods will be used to communicate with payers, physicians, and health systems?
- How will we document effects and impact of MTM in the practice?
- Pharmacist and technician time
- Changes in patients' medications, outcomes
- Other impact on pharmacy practice
|
| Figure 3. Medication Therapy Management Flowchart |
 |
What does the future hold for technicians in MTM services?
With continued changes in healthcare policy we can expect many aspects of MTM to evolve. This may include more ways in which pharmacists can receive payment for MTM services. Changes in legislation may continue to expand the reimbursement options available to pharmacists for MTM services. An official statement by the American Society of Health–System Pharmacists (ASHP) about the roles of pharmacy technicians states:21
"Pharmacy technicians have important roles and responsibilities in the pharmacy profession...A safe and effective medication–use process depends significantly on the [technicians'] skills, knowledge, and competence."
Conclusion
Now is an ideal time for pharmacy technicians who are not already involved in MTM to begin learning about the process. There is growing recognition by pharmacists that technician support is essential for successful and efficient MTM—and that appropriate technician training is needed. Pharmacy technicians who are aware of MTM principles and how they can support the MTM process will be in a good position to meet the changing needs of the pharmacy profession.
References
- Patient-Centered Primary Care Collaborative. The Patient-Centered Medical Home: Integrating Comprehensive Medication Management to Optimize Patient Outcomes. Resource Guide, 2nd ed. June 2012. Available at: http://www.pcpcc.org/sites/default/files/media/medmanagement.pdf.
- Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA). Cost and Utilization Management; Quality Assurance; Medication Therapy Management Program. Pub L No. 108-173, 117 Stat 2070.
- Centers for Medicare & Medicaid Services (CMS). A Physician's Guide to Medicare Part D Medication Therapy Management (MTM) Programs. MLN Matters Number SE1229.
- Centers for Medicare & Medicaid Services. 2017 Medicare Part D Medication Therapy Management (MTM) Programs. Fact Sheet: Summary of 2017 MTM Programs. August 16, 2017. Available at: https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/CY2017-MTM-Fact-Sheet.pdf
- IMS Institute for Health Informatics. The Use of Medicines in the United States: Review of 2011. April 2012.
- Center for Medicare and Medicaid Services (CME) National Health Expenditure (NHE) Fact Sheet. Updated 6/14/2017. Available at: www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nhe-fact-sheet.html
- Anderson GF. Testimony before the Senate Special Committee on Aging. The Future of Medicare: Recognizing the Need for Chronic Care Coordination. Serial No. 110-7. May 9, 2007, pp 19-20.
- Boparai MK, Korc-Grodzicki B. Prescribing for older adults. Mt Sinai J Med. 2011;78(4):613-626.
- Hanlon JT, Shimp LA, Semla TP. Recent advances in geriatrics: drug-related problems in the elderly. Ann Pharmacother. 2000;34(3):360-365.
- Pasina L, Brucato AL, Falcone C, et al. Medication non-adherence among elderly patients newly discharged and receiving polypharmacy. Drugs Aging. 2014;31(4):283-289.
- Tamura BK, Bell CL, Inaba M, et al. Outcomes of polypharmacy in nursing home residents. Clin Geriatr Med. 2012;28(2):217-236.
- Ernst FR, Grizzle AJ. Drug-related morbidity and mortality: updating the cost-of-illness model. J Am Pharm Assoc. 2001;41(2):192-199.
- American Pharmacists Association and the National Association of Chain Drug Stores Foundation. Medication Therapy Management in Pharmacy Practice: Core Elements of an MTM Service Model. Version 2.0. 2008.
- Giberson S, Yoder S, Lee MP. Improving Patient and Health System Outcomes Through Advanced Pharmacy Practice. A Report to the U.S. Surgeon General. Office of the Chief Pharmacist. U.S. Public Health Service. Dec 2011.
- California Pharmacists Association. Expanding Pharmacist Services: What Does This Mean for Me? Updated 2017. Available at: http://www.cpha.com/Advocacy/Expanding-Pharmacist-Services
- H.R. 592 - Pharmacy and Medically Underserved Areas Enhancement Act. Congress.gov. Introduced 01/20/2017. Available at: https://www.congress.gov/bill/115th-congress/house-bill/592
- Centers for Medicare & Medicaid Services (CMS). CY 2014 Medication Therapy Management Program Guidance and Submission Instructions. April 5, 2013.
- Isetts BJ, Schondelmeyer SW, Artz MB, et al. Clinical and economic outcomes of medication therapy management services: the Minnesota experience. J Am Pharm Assoc. 2008;48(2):203-213.
- Smith M, Giuliano MR, Starkowski MP. In Connecticut: improving patient medication management in primary care. Health Aff (Millwood). 2011;30(4):646-654.
- Stebbins MR, Cutler TW, Parker PL. Assessment of Therapy and Medication Therapy Management. In: Alldredge BK, Corelli RL, Ernst ME, et al. Koda-Kimble and Youngs Applied Therapeutics: The Clinical Use of Drugs. 10th ed. Baltimore: Wolters Kluwer/Lippincott Williams & Wilkins; 2013.
- American Society of Health-System Pharmacists. ASHP Statement on the Roles of Pharmacy Technicians. Am J Health-Syst Pharm. 2016; 73:928–930. Available at: https://www.ashp.org/-/media/assets/policy-guidelines/docs/statements-roles-of-pharmacy-technicians.ashx?la=en.
Back to Top