
Expired activity
Please go to the PowerPak
homepage and select a course.
Treatment Challenges in Acute Lymphoblastic Leukemia: Pharmacists' Key Role in Ensuring Best Practices
INTRODUCTION
Acute lymphoblastic leukemia (ALL) is an aggressive type of leukemia characterized by the monoclonal proliferation and expansion of immature lymphoid cells in the bone marrow and peripheral blood.1 It can also spread to the central nervous system (CNS), liver, lymph nodes, spleen, and other organs. In 2018, an estimated 5960 cases of ALL will be diagnosed in the United States (U.S.), and approximately 1470 deaths will occur from this disease.2 Most of the deaths that occur will be in adults. ALL is most commonly diagnosed in children, with 57% of patients diagnosed at an age younger than 20 years old. It is the most common leukemia in children and the least common leukemia among adults.1
Risk factors for developing ALL include age older than 70 years, exposure to chemotherapy or radiation therapy, and genetic disorders, such as Down Syndrome.3 Without treatment, ALL progresses very quickly, and survival is largely affected by whether a patient relapses.4 Although cure rates and survival outcomes have dramatically improved in recent years, most of these improvements are seen in children. The overall survival (OS) rate in pediatric ALL is approximately 86% to 89%.3 The OS rate decreases in young adults (age 15-39 years) to 42% to 63%, and, for adults (age 40 years and older), 5-year survival rates are only 17% to 24%. Age at diagnosis (30 to 35 years), white blood cell (WBC) count less than 50 x 109 cells/L, short time interval to achieve complete remission (CR), and certain cytogenetic abnormalities are associated with a better prognosis.
These cure rates demonstrate that OS decreases substantially with age, and, thus, children, young adults, and adults are treated differently. This monograph will focus on ALL in adult patients (age 40 years and older).
ALL is not a single disease but, rather, a group of related diseases that can be broadly classified into 3 subtypes: precursor B-cell ALL, mature B-cell ALL, and T-cell ALL. These different subtypes dictate different responses to treatment and outcomes. Roughly three-quarters of adult ALL cases are B-cell subtypes and the remaining one-quarter are the T-cell subtype.3 Each ALL subtype is associated with a different prognosis, but other factors (e.g., mutation status) may impact an individual patient's response to treatment and outcomes. Risk stratification on the basis of prognostic factors allows the healthcare team to determine the most appropriate initial treatment and to decide when to consider allogeneic stem cell transplantation in the treatment paradigm.5
Treatment of ALL is complex and the optimal management of acute ALL is especially challenging in adults. Frontline treatment of ALL may involve multiple chemotherapy or targeted agents administered in a sequential series along a several-year timeline (Figure 1).5,6 Typically, treatment begins with a 1-month induction chemotherapy regimen with CNS prophylaxis. The goal of this regimen is achieving CR. Once CR is achieved, a 4- to 6-month period of intensification chemotherapy without CNS prophylaxis occurs, with the goal of suppressing drug-resistant leukemic cells. Finally, maintenance therapy with oral anticancer agents commences for 18 to 24 months to prevent late relapse. Overall, 85% to 90% of adults with ALL achieve CR status following appropriate induction therapy. Adults who relapse after frontline therapy have extremely poor outcomes despite advances in chemotherapy and hematopoietic stem cell transplantation (HSCT). While up to 90% of adults respond to induction chemotherapy, only 30% to 40% will achieve long-term remission.
| Figure 1. Diagnosis and Treatment of Acute Lymphoblastic Leukemia6 |
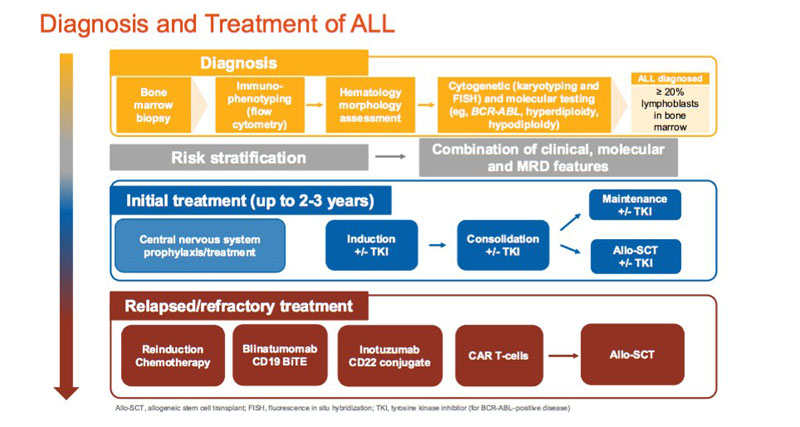 |
| Reprinted with permission from Dr. Patrick Brown, Johns Hopkins University School of Medicine. |
New treatments and approaches may confer benefits in adults and patients with relapsed/refractory disease. Novel targeted therapies, such tyrosine kinase inhibitors (TKIs) and monoclonal antibodies, have been shown to improve outcomes in adults with ALL. Additionally, antibody-drug conjugates (ADCs) represent a major advance in the treatment of ALL. ADCs employ 2 important treatment principles: antibody specificity for the tumor antigen and toxicity from the attached cytotoxic drug. Most recently, chimeric antigen receptor (CAR) T-cell therapy has been approved, which harnesses the patient's own immune system to attack the leukemia.
Pharmacists have important roles in caring for patients with ALL, including effective patient selection, treatment planning, and adverse effect and drug-drug interaction management. This activity provides an update for pharmacists on treatment options and approaches to supporting optimal outcomes in adult patients with relapsed/refractory ALL.
