
Expired activity
Please go to the PowerPak
homepage and select a course.
Vaccination Needs in the Older Adult: The Pharmacist's Role
"Hi," Henry said to the girl at the register, setting his basket on the pharmacy counter and unloading an assortment of day and night cold and flu medicine, cough syrup, throat lozenges, aspirin, vitamin C, echinacea, mentholated rub, hand sanitizer, toilet paper and bismuth subsalicylate.
"Hi," she chirped. "Have you gotten your flu shot yet?"
"No." He stepped back and dug for his wallet. "Not interested."
"Oh, but you should be! We're recommending it for all our senior citizens." She turned and waved over a woman in a lab coat. "Our pharmacist would be happy to answer any questions you might have."
"Thanks, but I don't have any," he said with a brief, forced smile. "I just don't want one."
"I know, my grandparents hate needles, too, but they both swore it didn't hurt at all." Her voice, soft with sympathy, perked back up. "And it was free for them and you'd probably get it for free, too."
"I'm not afraid of needles." And feeling suddenly trapped beneath the combined weight of their bright, earnest gazes, he added, "My buddy got one last year and it gave him the flu. He was sick as a dog; fever, chills, nonstop puking, diarrhea…"
The pharmacist frowned. "That sounds more like a stomach bug than—"
"He was laid up for weeks," he continued, knowing they didn't get it. "I mean, we were in 'Nam together, we've seen some stuff and he still said that shot really took it out of him." He shook his head. "It was so bad that his wife had to help him to the bathroom because he couldn't even get out of bed on his own. So, no, I'll pass." He gestured at his purchases. "What do I owe you?"
He remained firm in his refusal, enduring the register girl's silent disapproval as she rung him up and the pharmacist's dogged explanation of the shot itself and why someone in his age bracket should consider it an important preventative measure.
"Thanks, but no thanks," he said and when he'd finally left with his bags of OTC medicines thudding against his legs, he knew they'd written him off as a stubborn old coot with an unreasonable suspicion of modern medicine.
That was fine. Easier than trying to explain how he'd grown up in a different time, lived a very different life, had somehow become frail and sometimes fearful in ways he'd never seen coming and if there was even a chance that shot could give him the flu, he couldn't risk it. Wouldn't be fool enough to invite it into his body because he didn't have the luxury of being sick in bed anymore.
Didn't have the comfort of feeling safe, knowing someone was always there, caring for him.
Henry's wife had passed, and his kids were gone. There was no one left in his house but him.
Introduction and Epidemiology Attributed to Vaccine-Preventable Disease
The aging global population demands healthcare systems throughout the world evaluate initiatives to ensure healthy aging and optimization of preventative health strategies for this population. By the year 2050, it is estimated more than 2.1 billion individuals around the world will have reached 60 years or older.1 Notably, the number of individuals above 80 years of age is expected to increase from a worldwide total of 125 million in 2015 to a staggering 434 million by 2050.2 Infectious disease prevention, including vaccination strategies targeting individuals at various stages of life, is a critical public health measure to ensure optimization of quality of life and health maintenance regardless of age.
Vaccination represents an important aspect of preventative health, particularly for older adults. Individuals aged 65 years or older are a susceptible population, at higher risk for complications of vaccine-preventable illnesses and death from potentially preventable infectious diseases. Vaccination against communicable diseases, such as influenza and pneumococcal disease, is an invaluable yet often underestimated and underutilized healthcare tool that can decrease morbidity and mortality in older adults.
Based on a report of the National Vaccine Advisory Committee, more than 40,000 older adults die annually in the United States (US) from vaccine-preventable illnesses.3 Increasing the rate of vaccinations among older adults is a priority of the US government addressed in the Healthy People 2020 initiative.4
| Older adults are at increased risk for serious complications from vaccine-preventable illnesses due to age-associated changes in immune function and chronic medical comorbidities; both of which place them at a higher risk for infection and for having an infection with a protracted course.5 |
Vaccination rates among older adults remain low despite well-established guidelines and endorsement by many professional organizations. Approximately 74% of older adults received the influenza vaccination during the 2015 influenza season; 64% of older adults have received any pneumococcal vaccination as of 2015; and only 27.9% of eligible older adults reported receiving the herpes zoster vaccine in 2014.6
| There remains a tremendous opportunity for healthcare professionals, including primary care providers and pharmacists, to influence these low rates of vaccine uptake, to educate the public on recommended vaccinations according to age and presence of medical comorbidities, and to prevent potentially communicable disease transmission and associated complications among older adult patients. |
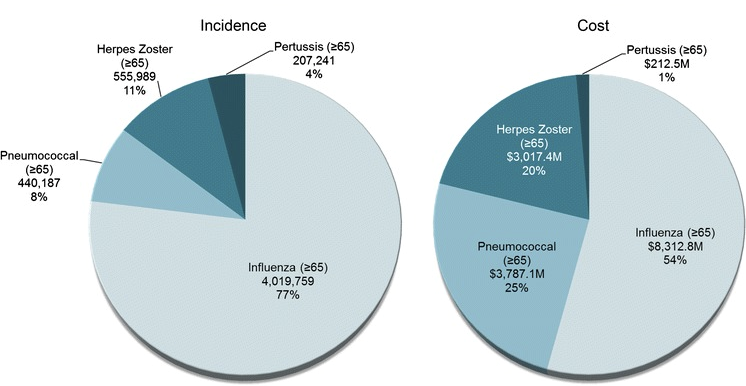
In a healthcare environment characterized by limited resources and a rapidly increasing elderly population, it is critical to explore preventative health interventions to ensure appropriate use of healthcare dollars where possible. Of the $26.5 billion total estimated treatment cost of adult vaccine-preventable disease in the US among adults aged 50 and older, $15.3 billion (58%) was attributable to care for adults 65 and older (Figure 1).5 According to the Centers for Disease Control and Prevention (CDC), low uptake of routinely recommended adult immunizations remains one area of public health practice that has been insufficiently addressed at local, state, and national levels.6
Figure 1. Percentage of estimated cases of vaccine preventable illness and estimated cost of vaccine preventable illness7
In this activity, age-associated changes in immunologic function will be explored. Current vaccination recommendations specifically for influenza, pneumococcal and herpes zoster-containing vaccines in the older adult population will be reviewed, and the role of the pharmacist in ensuring optimization of immunization uptake in the older adult population elucidated.
