
Expired activity
Please go to the PowerPak
homepage and select a course.
Chronic diseases are the leading cause of death and disability in the United States. People are living longer with chronic diseases, which often means that they require complex medical treatment over a period of many years. People with chronic diseases tend to take multiple medications, have overlapping medical conditions, and have an increasing risk of disease– related complications and medication side effects as they age. Improving the management of chronic diseases is the major focus of medication therapy management (MTM). Pharmacy technicians work regularly with patients who have chronic diseases. In most practice settings, people with chronic diseases are the main population receiving MTM services. One reason why improving care for these patients is so important is that many chronic diseases— and their complications—are mostly or partly preventable. Improved management of chronic diseases can help reduce hospitalizations, disability, missed time from work and family responsibilities, and overall healthcare costs.
IMPACT OF CHRONIC DISEASE IN THE U.S.
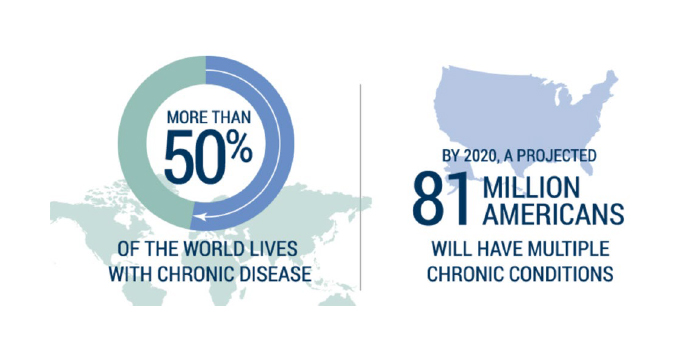
Chronic diseases are a growing concern worldwide—even in parts of the world facing issues such as infectious diseases, malnutrition, and maternal/child mortality.1 In the U.S., chronic diseases are the major health threat. Half of all adults—about 117 million people—have at least one chronic health condition, while about 25% of adults have two or more chronic health conditions.2
Seven of the top 10 causes of death are chronic diseases, including heart disease, chronic obstructive pulmonary disease (COPD), cancer, stroke, Alzheimer’s disease, diabetes, and chronic kidney disease. The top two chronic diseases (heart disease and cancer) make up nearly half of all deaths (Figure 1).3
| Figure 1. Leading Causes of Death, United States, 2018 (Thousands; 000)3 |
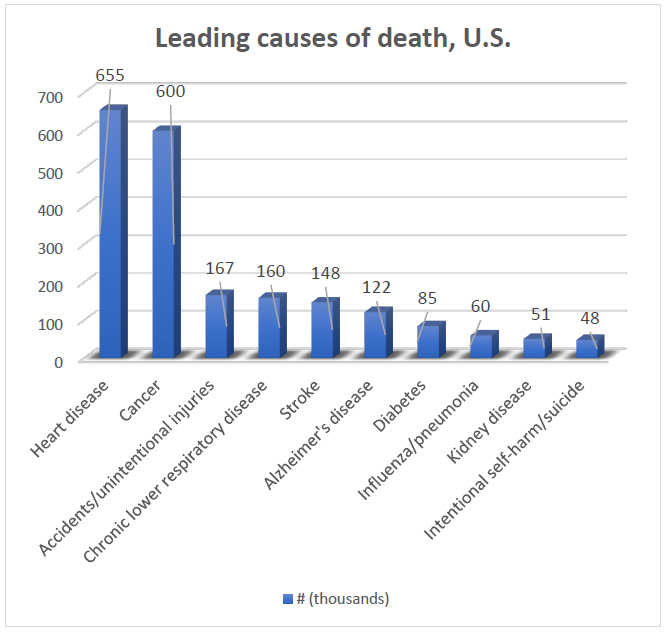 |
| Source: Centers for Disease Control and Prevention. National Center for Health Statistics.3 |
Chronic diseases are a common cause of death, but also carry a burden of illness and disability for individuals living with these conditions. Some diseases that may not be significant causes of death—such as arthritis—are associated with high levels of disability.4,5 And, both men and women with heart disease are surviving longer, as shown in the chart in Figure 2.6 Longer survival times from chronic disease, combined with increasing risk factors, means that the number of people affected (the prevalence) increases each year.
Figure 2. Declining Deaths from Cancer and Heart Disease
Men and women, 1980 to 2010 |
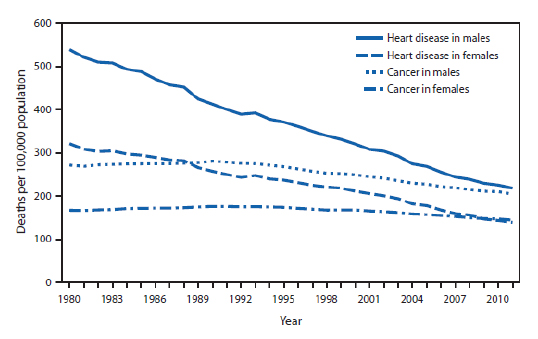 |
| Source: Centers for Disease Control and Prevention. Morbid Mortal Wkly Rep.6 |
HOW LIFESTYLE AND BEHAVIORAL FACTORS AFFECT CHRONIC DISEASE
The technical definition of “chronic disease” is a disease that lasts three months or longer.7 Other definitions describe chronic disease as a condition that is considered long–term or permanent (incurable) and one that cannot be prevented by vaccines or cured by medications.)2 Many chronic diseases are partly or even mostly preventable. The diagram below from a World Health Organization (WHO) report on chronic disease shows how modifiable (e.g., unhealthy diet, too little exercise) and non–modifiable (e.g., age, heredity) risk factors lead to common chronic diseases (Figure 3).8
| Figure 3. Impact of Risk Factors on Chronic Diseases8 |
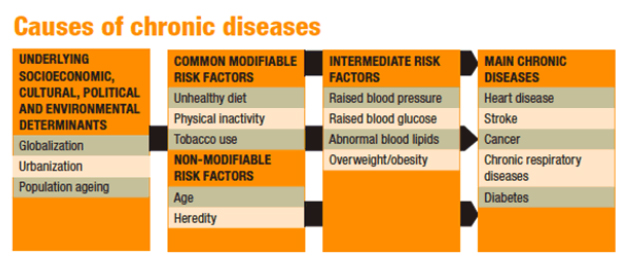 |
| Source: World Health Organization. Preventing Chronic Diseases: A Vital Investment. WHO Global Report.8 |
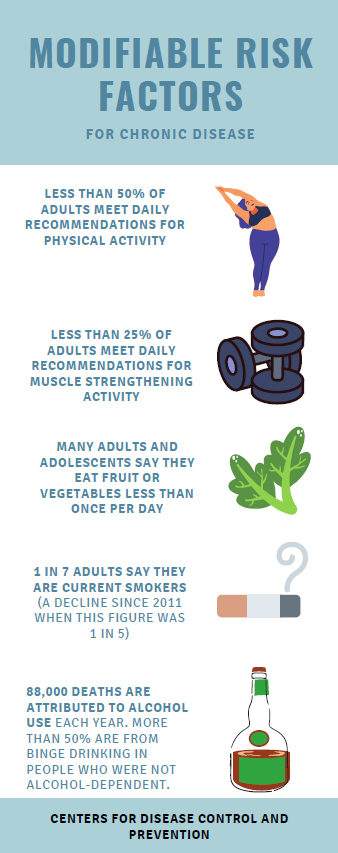 The four key modifiable risk factors associated with most of the disability and death due to chronic disease are:9
The four key modifiable risk factors associated with most of the disability and death due to chronic disease are:9
1) Unhealthy diet
2) Lack of exercise
3) Smoking or other tobacco use
4) Excessive alcohol use
Unhealthy lifestyle choices lead to intermediate risk factors such as high blood pressure, high blood sugar, high cholesterol levels, and excess weight or obesity. These risk factors are treatable, and intervention combined with steps toward improving lifestyle can prevent and even reverse the effects of chronic diseases. However, these problems are complex and are rarely “easy fixes.” Obesity is an underlying factor in many chronic diseases in this country, with rates of obesity among adults and children rapidly climbing. The maps in Figure 4 that both obesity (left) and diabetes (right) are widespread in the U.S., particularly in the Southeastern states.10 Obesity is a major risk factor for heart disease, cancer, stroke, diabetes, and kidney disease—as well as joint injuries, stress–related illness, fertility problems, and many other health conditions.
| Figure 4. Obesity and Diabetes Across America10 |
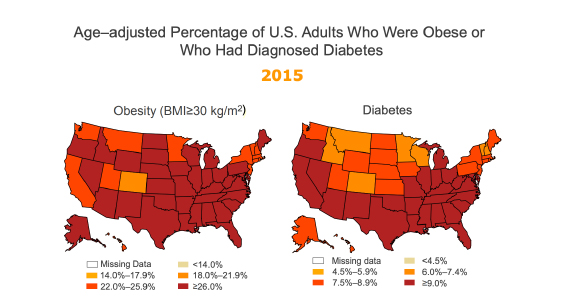 |
| Source: Centers for Disease Control and Prevention. Maps of Trends in Diagnosed Diabetes and Obesity, 2017.10 |
CHRONIC DISEASES AND MEDICARE PART D COVERAGE OF MTM
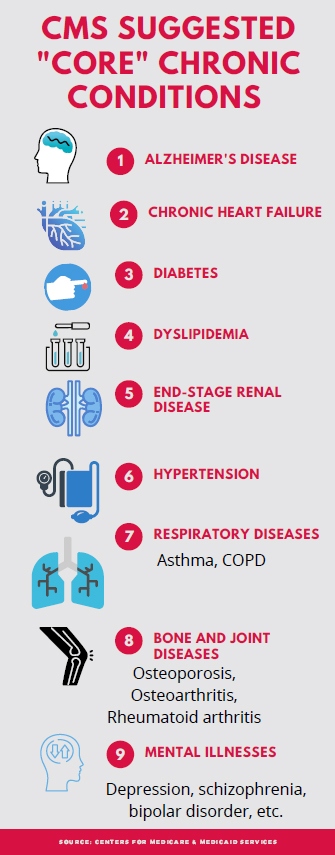 Pharmacy technicians who participate in MTM will need to understand the Core Chronic Disease States that qualify for coverage of MTM services under Medicare Part D.
Pharmacy technicians who participate in MTM will need to understand the Core Chronic Disease States that qualify for coverage of MTM services under Medicare Part D.
Medicare Part D “sponsors” are private insurance/managed care companies that provide drug benefits to people enrolled in Medicare Part D. To try to lower drug costs and better manage disease, Medicare will reimburse these organizations for the cost of MTM services. Some sponsors offer their own MTM services (often via telephone). Or they may contract with pharmacies to provide MTM services. Patients who receive MTM services under Medicare Part D must meet certain criteria, as outlined below.
For automatic enrollment (eligibility) in MTM, patient must meet all 3 criteria:11
1. Two or more chronic diseases
(Some sponsors may be more lenient and extend MTM services for patients with one chronic disease.)
The sponsor may elect to cover MTM for any set of chronic diseases, but they must include at least 5 of the 9 “core” chronic conditions listed below:
2. Use of multiple drugs (covered by Medicare Part D)12
Each Medicare Part D sponsor determines the specific drugs covered under its formulary. The number of prescription drugs the patient must be taking to quality for MTM usually ranges between 2 and 8. (Sponsors cannot require that patients be taking more than 8 drugs to qualify for MTM services.)
3. High annual medication costs12
For the year 2020 the amount set by CMS was $4,255 or higher. The sponsors look at first–quarter drug spending to estimate the likelihood of a patient spending this amount over a year. (This amount is adjusted by CMS each year.) Some prescription drug plans have set a higher threshold for the annual drug costs in order for the patient to qualify for MTM.
HOW CAN MTM HELP IN THE MANAGEMENT OF CHRONIC DISEASES?
There are many examples of research showing that pharmacist–provided MTM services can have positive, tangible effects on the management of chronic diseases. Diabetes is one of the most prominent disease states in which research has been done. Studies have shown that, compared with usual care, patients receiving MTM (or similar services) are more likely to reach treatment goals for diabetes such as target hemoglobin (HbA1c) levels and to have higher medication adherence rates.
- A study conducted at Vanderbilt University showed that medically underserved patients with uncontrolled diabetes who received pharmacist–provided MTM services had higher rates of medication adherence, lower A1C levels, and lower LDL cholesterol levels.13
- A Minnesota study compared the long–term effects of pharmacist–led MTM services with standard care in patients with diabetes. The percentage of diabetes patients who were optimally managed was significantly higher in the group receiving MTM. MTM patients were more likely to meet the HbA1c criteria and had greater overall reductions in HbA1c.14
A study of the effects of MTM in multiple disease states was conducted in Connecticut, in which 9 pharmacists worked closely with 88 Medicaid patients between over a one-year period to conduct MTM services. During that year:15
- 369 patient–pharmacist encounters were analyzed
- 917 drug therapy problems were identified by pharmacists
- 78% of problems were resolvedwithout referring patient back to primary care provider
- 82% of prescribers made changes in therapy based on pharmacists’ recommendations
Table 1 summarizes benefits of pharmacist–provided MTM services on health outcomes for patients with chronic diseases such as heart failure, diabetes, hypertension, and dyslipidemia.
| Table 1. Benefits of MTM in Selected Health Outcomes |
| Disease state/condition |
# patients (# studies)
Source |
Outcome/effect of pharmacist intervention |
| Diabetes |
2,247 (16)16 |
Significantly reduced HbA1c levels |
Diabetes
(10-City Challenge) |
573 (1 multicenter)17 |
Influenza vaccination rate doubled; eye and foot examination rates increased |
Diabetes
(Asheville Project) |
12 community pharmacies followed for 5 years18,19 |
Significantly reduced mean HbA1c; increased % of patients with optimal A1c; improved lipid levels; decreased costs of care; decreased sick days |
| Hypertension |
2,246 (13)16 |
Significantly reduced systolic blood pressure |
| Multiple chronic conditions |
Connecticut Medicaid Project15,20 |
917 drug therapy problems identified in 369 pharmacist/patient encounters; pharmacists resolved 78% without additional physician visit |
MTM FOR CHILDREN WITH CHRONIC DISEASES
Chronic diseases are not just among older adults. Increasingly, children are living with chronic diseases, especially conditions associated with environmental causes (such as asthma) and lifestyle (such as diabetes). There are many circumstances in which MTM can be beneficial for parents of children with chronic disease. An example might be a child who has frequent emergency room visits and/or excessive use of rescue medications for asthma.21 MTM counseling can help the parent (or adolescent) to better understand the purpose of asthma maintenance therapies.22 Other examples would be children with juvenile rheumatoid arthritis, or HIV/AIDS, which require complex regimens utilizing high–cost specialty drugs.23,24
Childhood obesity is a growing public health concern:25
- Currently one in 3 children are overweight.
- About 18.5% of all U.S. children and adolescents aged 2 to 19 years are obese;
- These rates are higher among Hispanic children/adolescents (22%) and Black children/adolescents (20%).
Type 2 diabetes used to occur only rarely in children, but now represents almost half of all childhood diabetes diagnoses.26 Diabetes among overweight and obese children is a particular problem among black and Hispanic populations.27,28 Studies show that children with diabetes have poor medication adherence and poor glucose control, and that diabetes tends to progress faster in younger patients.29 Thus pharmacist–provided MTM targeted at parents and teens/adolescents with diabetes may help establish lifestyle changes and patterns to help them manage this complex condition.
CONCLUSION
An understanding of chronic diseases and the magnitude of the problem is especially important in the practice of MTM. Pharmacy technicians may interact frequently with these patients and should have an appreciation of the potential for MTM to aid in chronic disease management.
REFERENCES
- World Health Organization. Noncommunicable diseases. June 1, 2018. Available at: https://www.who.int/en/news-room/fact-sheets/detail/noncommunicable-diseases.
- Center for Managing Chronic Disease. Putting People at the Center of Solutions. University of Michigan, 2020. Available at: https://cmcd.sph.umich.edu/.
- Centers for Disease Control and Prevention. National Center for Health Statistics. Leading Causes of Death, U.S. Chronic Disease Prevention and Health Promotion. Updated Oct 2020. Available at: https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm.
- Sandoval-Rosario M, Nayeri BM, Rascon A, et al. Prevalence of Arthritis Among Adults with Prediabetes and Arthritis-Specific Barriers to Important Interventions for Prediabetes - United States, 2009-2016. MMWR Morb Mortal Wkly Rep. 2018;67(44):1238-1241.
- Barbour KE, Helmick CG, Boring M, et al. Prevalence of Doctor-Diagnosed Arthritis at State and County Levels - United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(19):489-494.
- Centers for Disease Control and Prevention. QuickStats: Age-adjusted death rates for heart disease and cancer, by Sex – United States, 1980-2011. Morbid Mortal Wkly Rep. Sept 19, 2014. Available at: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6337a6.htm.
- Goodman RA, Posner SF, Huang ES, et al. Defining and measuring chronic conditions: imperatives for research, policy, program, and practice. Prev Chronic Dis. 2013;10:E66.
- Source: World Health Organization. Preventing Chronic Diseases: A Vital Investment. WHO Global Report. Available at: https://www.who.int/chp/chronic_disease_report/en/.
- Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP). Fact Sheets and At a Glances. Updated Sept 18, 2020. Available at: https://www.cdc.gov/chronicdisease/resources/publications/aag.htm.
- Centers for Disease Control and Prevention. Maps of Trends in Diagnosed Diabetes and Obesity. 2017. Availablle at: https://www.cdc.gov/diabetes/statistics/slides/maps_diabetesobesity_trends.pdf.
- Centers for Medicare & Medicaid Services (CMS). Medicare Part D Medication Therapy Management Program Standardized Format. Form CMS-10396_08/17. Available at: https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/MTM.
- National Community Pharmacists Association (NCPA). Medicare Part D 2020 Fact Sheet. http://www.ncpa.co/pdf/part-D-2020-fact-sheet.pdf.
- Skinner JS, Poe B, Hopper R, et al. Assessing the effectiveness of pharmacist-directed medication therapy management in improving diabetes outcomes in patients with poorly controlled diabetes. Diabetes Educ. 2015;41(4):459-465.
- Brummel AR, Soliman AM, Carlson AM, et al. Optimal diabetes care outcomes following face-to-face medication therapy management services. Popul Health Manag. 2013;16(1):28-34.
- Smith SB, Mango MD. Pharmacy-based medication reconciliation program utilizing pharmacists and technicians: a process improvement initiative. Hosp Pharm. 2013;48(2):112-119.
- Machado M, Nassor N, Bajcar JM, et al. Sensitivity of patient outcomes to pharmacist interventions. Part III: systematic review and meta-analysis in hyperlipidemia management. Ann Pharmacother. 2008;42(9):1195-1207.
- Fera T, Bluml BM, Ellis WM. Diabetes Ten City Challenge: final economic and clinical results. J Am Pharm Assoc (2003). 2009;49(3):383-391.
- Cranor CW, Bunting BA, Christensen DB. The Asheville Project: long-term clinical and economic outcomes of a community pharmacy diabetes care program. J Am Pharm Assoc (Wash). 2003;43(2):173-184.
- Bunting BA, Cranor CW. The Asheville Project: long-term clinical, humanistic, and economic outcomes of a community-based medication therapy management program for asthma. J Am Pharm Assoc (2003). 2006;46(2):133-147.
- Smith M, Giuliano MR, Starkowski MP. In Connecticut: improving patient medication management in primary care. Health Aff (Millwood). 2011;30(4):646-654.
- Al-Muhsen S, Horanieh N, Dulgom S, et al. Poor asthma education and medication compliance are associated with increased emergency department visits by asthmatic children. Ann Thorac Med. 2015;10(2):123-131.
- Frey SM, Fagnano M, Halterman JS. Caregiver education to promote appropriate use of preventive asthma medications: what is happening in primary care? J Asthma. 2016;53(2):213-219.
- Kibicho J, Dilworth T, Owczarzak J, et al. Pharmacist-initiated adherence promotion activities for persons living with HIV in ambulatory care settings: Instrument development and initial psychometric testing. Res Social Adm Pharm. 2020;16(7):921-927.
- Len CA, Miotto e Silva VB, Terreri MT. Importance of adherence in the outcome of juvenile idiopathic arthritis. Curr Rheumatol Rep. 2014;16(4):410.
- Centers for Disease Control and Prevention. Childhood Obesity Facts. Updated June 24, 2019. Available at: http://www.cdc.gov/obesity/data/childhood.html.
- D'Adamo E, Caprio S. Type 2 diabetes in youth: epidemiology and pathophysiology. Diabetes Care. 2011;34 Suppl 2(Suppl 2):S161-165.
- Mayer-Davis EJ, Lawrence JM, Dabelea D, et al. Incidence Trends of Type 1 and Type 2 Diabetes among Youths, 2002-2012. N Engl J Med. 2017;376(15):1419-1429.
- Reynolds K, Saydah SH, Isom S, et al. Mortality in youth-onset type 1 and type 2 diabetes: The SEARCH for Diabetes in Youth study. J Diabetes Complications. 2018;32(6):545-549.
- Gonzalez JS, Tanenbaum ML, Commissariat PV. Psychosocial factors in medication adherence and diabetes self-management: Implications for research and practice. Am Psychol. 2016;71(7):539-551.