
Expired activity
Please go to the PowerPak
homepage and select a course.
Medication therapy management (MTM) is particularly appropriate for older patients. As people age, they are at risk for a greater number of chronic health conditions. Older people also use more medications, have more hospitalizations, see more physicians, and are more likely to have factors (such as dementia, memory problems, or visual problems) that affect their ability to take medications correctly. In addition, people's bodies respond differently to many medications as they age. MTM can help toward the goal of individually tailoring medical treatments for the individual, taking into account the physical and social changes associated with aging.
FACTS ABOUT THE AGING POPULATION
The aging of the U.S. population has been widely discussed in healthcare settings. Statistics show that the proportion of the population over age 65 has been steadily climbing. In the century from 1960 to 2060, the population is projected to look much more like a "cylinder" than an "pyramid," with a larger proportion of the population at many of the older age groups, as shown in Figure 1.1
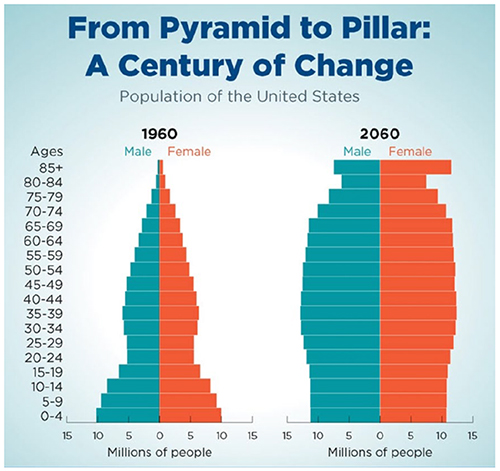
| Figure 1. U.S. Population Distribution by Age, 1960 vs Projected Population in 2060 |
 |
| Source: U.S. Census, National Population Projections, 2017.1 |
The statistics cited above illustrate how healthcare will continue to be influenced in the coming decades by an aging population. To save costs, CMS has increased pressure on hospitals to shift older hospitalized patients to long–term care settings more quickly, and in 2017 altered its payment structure to reflect this shift toward long–term care.2
Who are the "oldest old"?
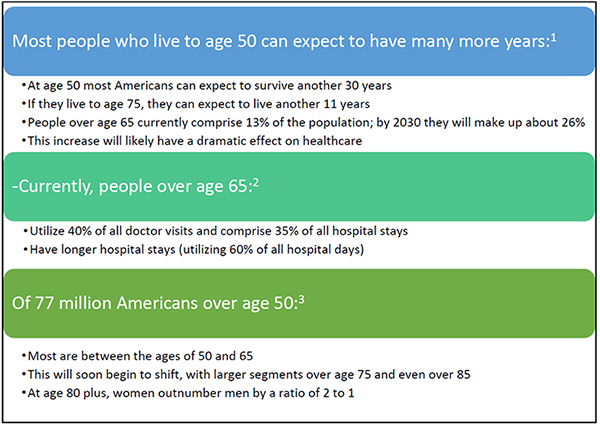
The oldest old (age 85 years and up) make up the fastest–growing segment of the population. According to the World Health Organization (WHO), the number of people aged 85 and older living in developed countries is expected to increase by 351% from 2010 to 2050.3 This is compared with just a 22% increase in the group under age 65 during that time period. Coming across "centenarians"—people who have lived past the 100–year mark— is no longer a rare event. In the U.S., there are about 53,000 centenarians.4 Women make up over 80% of the centenarian population.3
| Figure 2. Percent Increase in "Oldest Old" Age Segments from 2010 to 20503 |
 |
| Source: World Health Organization, National Institutes of Health. Global Health and Aging. NIH Publication 11-7737.3 |
GERIATRIC SYNDROMES
Many chronic diseases are more common in older people. According to the 2008 National Health Interview Survey:5
- 78% of adults age 55 and older had 1 or more chronic health conditions;
- 47% had 2 or more chronic health conditions;
- 19% had 3 or more chronic health conditions.
Healthcare costs for individuals with at least 3 chronic conditions accounted for 89% of Medicare's annual budget. Comorbidity is associated with poor quality of life, physical disability, high healthcare use, multiple medications, and increased risk for adverse drug events and mortality.6,7
In addition to common chronic conditions like cardiovascular or lung diseases, many other age–related issues combine to affect the health of older adults. These conditions sometimes fall outside of the categories of "diseases," and are called "geriatric syndromes" (Table 1).8
|
Table 1. Common Geriatric Syndromes8
|
|
• Dementia
• Delirium (confused state)
• Urinary incontinence
• Falls
• Difficulty walking
• Dizziness
• Fainting
• Hearing impairment
• Visual impairment
• Osteopenia (reduced bone mass that occurs before osteoporosis)
• Malnutrition, poor diet, and eating/feeding problems
• Pressure sores
• Sleep disturbances
Other Geriatric Syndromes
• Polypharmacy (use of multiple medications)
• Neglecting self-care
• Elder abuse (abuse or neglect by caregivers or family members)
• Poor tolerance to extreme heat and cold
• Dehydration, electrolyte imbalance
• Misdiagnosis of illnesses and/or incorrect medical treatments
|
Medications can cause, mimic, or exacerbate a geriatric syndrome. An example might be a medication that causes lightheadedness, which may worsen an existing condition. There are four key characteristics that increase risk of geriatric syndromes. These are:
1) Older age
2) Baseline cognitive (mental) impairment
3) Baseline functional impairment (e.g., difficulty using the hands)
4) Impaired mobility (e.g., difficulty walking)
FRAILTY AND ITS EFFECT ON MEDICATION USE
Geriatric experts say that frailty is a more accurate predictor of geriatric syndromes than old age by itself.9Frailty has been defined as " impairment in mobility, balance, muscle strength, cognition, nutrition, endurance, and physical activity."10 Another source defines the term frail elderly as "older adults or aged individuals who are lacking in general strength and are unusually susceptible to disease or to other infirmity."11Advanced age does not necessarily determine whether a person is frail. There are many examples of people who live to highly advanced ages and seem healthy and vigorous, while others who are younger and have chronic diseases tend to progress to a frail state at much younger ages.
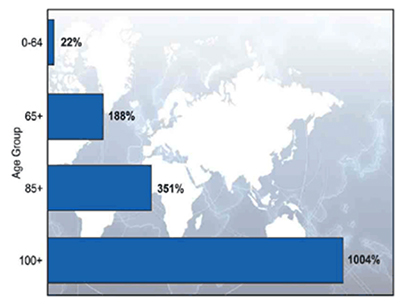
Advanced age and frailty combine to change how a person's body responds to medications. This includes changes in pharmacokinetics (how drugs are absorbed, metabolized and eliminated) and pharmacodynamics (how a drug acts in the body), as show in Figure 3.12,13
| Figure 3. Effects of Age on Pharmacokinetics and Pharmacodynamics12,13 |
 |
DRUGS AREN'T TESTED IN ELDERLY PATIENTS
Although medications behave differently in older individuals, unfortunately most medications are not tested in elderly patients. Drugs are brought to market using clinical trial protocols that rarely include older patients or those who take multiple medications or have multiple diseases. Therefore, drug trials do not reveal the types and frequency of adverse effect that are likely to occur in older patients, especially frail older patients. In addition, clinical practice guidelines for many disease states do not include discussion of how medications should be modified for the frail elderly.14-16 Many clinical practice guidelines only address one disease at a time, so the list of drugs recommended for the disease state does not take into account the fact that these people are taking other medications for multiple conditions.
Most other health challenges faced by older adults are also overlooked in clinical practice guidelines. These include having multiple doctors and pharmacies, frequent transitions of care, isolated living conditions, and difficulty performing activities of daily living.8,10
POLYPHARMACY AND OLDER ADULTS
Polypharmacy poses a greater hazard for older, frail patients, based on their diminished ability to eliminate medications and diminished physiological reserves. Impaired thinking and mental status can interfere with an elderly person's ability to manage multiple medications and complex dosing schedules, and to report when adverse events occur. As disease burden and decreased functional status progress, the elderly person becomes more isolated from support systems that can help them cope.17 Pharmacy technicians have a great deal of personal contact with the older patient and can be key to helping diminish the effects of this isolation.
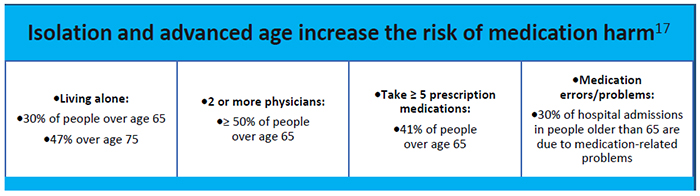
As noted in Module 7 on polypharmacy, adverse drug reactions may be mistaken for symptoms of diseases—this problem is more likely to occur in older patients.13,18 In addition, older patients may not report use of over–the–counter medications and supplements. One study showed that 30% of people over age 65 take analgesics regularly, but as many as 60% cannot identify the type of pain reliever they take.19 An estimated 40% of Americans believe that OTC medications are too weak to cause any real harm.19
MTM AND OLDER ADULTS
One of the chief goals of MTM is to provide medication management to older adults, including frail elderly patients, people with multiple chronic diseases, and those who take multiple medications. MTM offers the opportunity to take an individualized approach to each patient to increase the safety and effectiveness of medications for these patients. Important concepts to be explored in MTM by the pharmacist or pharmacy technician are outlined below and in Table 2. Documentation of this information will help the pharmacist perform more efficient and effective MTM consultations.
| Table 2. MTM Checklist for Technicians |
| □ Screen for health literacy |
• Does the person have difficulty or need help reading or understanding written or verbal instructions/educational materials?
• Use single-item literacy scale (SILS). (See Resources, Table 3)
|
| □ Ask about recent hospitalizations |
• When, where, why, and details on discharge (when, to where?)
|
| □ Determine number of prescribing healthcare providers |
• Gather contact information (regular providers, urgent care, specialty clinics, emergency department)
|
| □ Perform medication reconciliation |
• Obtain patient medication list, or ideally "brown bag" (patient brings in all Rx, OTC, herbals, supplements, and vitamins
• Include topical medications, suppositories)
• Ask which are currently being taken
• Note dates on bottles relative to current date
• Create current medication list
|
| □ Ask about sleep habits |
• Poor sleep habits could be related to medications, use of sleep aids, alcohol use
|
| □ Ask about eating habits |
• Medications could be affecting appetite
• Eating habits can affect how/when drugs are taken, disease states such as diabetes, etc.
|
| □ Determine barriers to obtaining medications |
• Insurance problems
• Coverage gaps
• Transportation problems
|
| □ Ask who manages the medications at home |
• Identify any caregivers
• If the caregiver manages medications, try to obtain contact information
|
When planning MTM services for an older adult, a few things to keep in mind are:
- Not all "elderly" people are the same. Aging is a highly diverse state. Different environmental exposures, disease states, genetics, and lifestyle choices influence a person's state of health as they age.13
- An older person's goals for medical treatment may differ from those of younger patients. If a "cure" is not possible, the goal of therapy for an older patient may be more palliative (helping them to be comfortable or feel better) rather than returning to normal function.
- Certain diseases may need to be treated less aggressively, in order to allow lower doses of medications and better tolerability. An example might be the hemoglobin A1c targets in diabetes. Treatment targets that are appropriate for a younger adult might not be advisable for a frail elderly person, and may actually reduce the patient's functional status by causing bouts of hypoglycemia.16
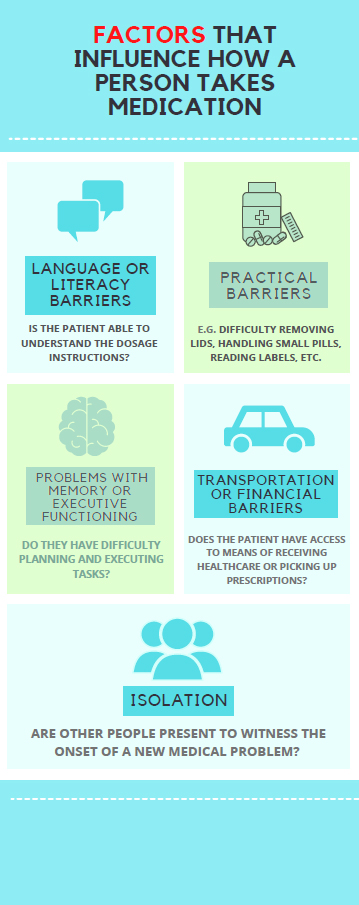
Social issues and effects of isolation
Social and personal issues affecting an individual are often overlooked by physicians when prescribing medications. MTM services can offer an opportunity to explore how such issues might be affecting how a person is taking his or her medications. Some issues to explore are shown in the graphic in Figure 4.
| Figure 4. Factors that May Affect How an Older Individual Takes Medications |
 |
Fall risk and older patients
It is also important for the pharmacy staff involved in MTM to be aware of the high risk of falls among older and frail individuals, and the impact of medications on fall risk. Medications associated with an increased risk of falls include benzodiazepines, muscle relaxants, antihistamines, antidepressants, and any others that cause dizziness, lightheadedness, or balance problems.20 Other factors that increase fall risk include neurologic changes that affect gait and balance (reduced ability to lift the leg, need to support the weight on both legs), poor eyesight, and physical deconditioning.21 Many falls in older patients simply are unreported and go undetected—the person does not want to "make a fuss" so may not report falls or cover up minor injuries. Falls are perceived as a sign that the person is growing more dependent, thus elderly patients may hesitate to report falls to family and physicians. Despite the high risk of falls, many people do not want to rely on assistive devices such as walkers or canes. The reasons given include 1) negative perceptions of "old age" and how other people may treat them; 2) a sign of "giving up" or accommodating to an illness; and 3) the idea that dependence on an assistive device will sacrifice needed exercise.22
CONCLUSION
MTM offers an excellent opportunity for medication review and management for older adults, but it is important to consider each person as an individual. "Elderspeak" is a term used for a habit of talking loudly in simple sentences, which may be insulting to the patient. Another habit is to speak to the adult son/daughter or caregiver, over the top of the elderly person's head. Pharmacy technicians who are participating in MTM should avoid these habits and address the individual patient according to his or her own needs. Individual needs should also be considered in regards to the effects of medications on the body (based on liver/kidney function, body weight, and other factors), cognitive abilities, and the person's social environment. Pharmacy technicians who are participating in MTM may take part in screening the patient for health literacy, reviewing the medication history, discussing medication use with the patient, and providing appropriate educational materials. It is important for the technician to be aware of the many factors that influence medication use in older adults.
REFERENCES
- U.S. Census. From Pyramid to Pillar: A Century of Change, Population of the U.S. March 13, 2018. National Population Projections, 2017. Available at: https://www.census.gov/library/visualizations/2018/comm/century-of-change.html.
- U.S. Department of Health and Human Services. Federal Register. 2016;81(162)56762–57438. Available at: https://www.gpo.gov/fdsys/pkg/FR–2016–08–22/pdf/2016–18476.pdf.
- World Health Organization, National Institutes of Health. Global Health and Aging. NIH Publication 11–7737. October 2011. Available at: http://www.who.int/ageing/publications/global_health.pdf.
- Kato K, Zweig R, Barzilai N, et al. Positive attitude towards life and emotional expression as personality phenotypes for centenarians. Aging (Albany NY). 2012;4(5):359-367.
- National Center for Health Statistics. Percentage of U.S. Adults 55 and Over with Chronic Conditions. Available at: https://www.cdc.gov/nchs/health_policy/adult_chronic_conditions.htm.
- Egede LE, Walker RJ, Bishu K, et al. Trends in Costs of Depression in Adults with Diabetes in the United States: Medical Expenditure Panel Survey, 2004-2011. J Gen Intern Med. 2016;31(6):615-622.
- McDaid D, Park A. Counting all the costs: the economic impact of comorbidity. In: Sartorius N, Holt RIG, Maj M (eds): Comorbidity of Mental and Physical Disorders. Basel: Karger, 2015, vol 179:23–32.
- Antimisiaris D, Cheek DJ. Polypharmacy. In: Mauk KL. Gerontological Nursing. Burlington, MA: Jones & Bartlett. 2014:417-456.
- Inouye SK, Studenski S, Tinetti ME, et al. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55(5):780-791.
- Antimisiaris DE. The elderly: medication use and prescribing issues. Polypharmacy Initiative, University of Kentucky. 2012.
- Bergman H, Ferrucci L, Guralnik J, et al. Frailty: an emerging research and clinical paradigm--issues and controversies. J Gerontol A Biol Sci Med Sci. 2007;62(7):731-737.
- Thürmann PA. Pharmacodynamics and pharmacokinetics in older adults. Curr Opin Anaesthesiol. 2020;33(1):109-113.
- Lonsdale DO, Baker EH. Understanding and managing medication in elderly people. Best Pract Res Clin Obstet Gynaecol. 2013;27(5):767-788.
- Boyd CM, Darer J, Boult C, et al. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. Jama. 2005;294(6):716-724.
- de Brantes F, Gosfield AG, McGlynn E, et al. Clinical practice guidelines for older patients with comorbid diseases. Jama. 2006;295(1):34; author reply 34-35.
- Munshi MN, Meneilly GS, Rodríguez-Mañas L, et al. Diabetes in ageing: pathways for developing the evidence base for clinical guidance. Lancet Diabetes Endocrinol. 2020;8(10):855-867.
- Marcum ZA, Amuan ME, Hanlon JT, et al. Prevalence of unplanned hospitalizations caused by adverse drug reactions in older veterans. J Am Geriatr Soc. 2012;60(1):34-41.
- Aspinall S, Sevick MA, Donohue J, et al. Medication errors in older adults: a review of recent publications. Am J Geriatr Pharmacother. 2007;5(1):75-84.
- Roumie CL, Griffin MR. Over-the-counter analgesics in older adults: a call for improved labelling and consumer education. Drugs Aging. 2004;21(8):485-498.
- Park H, Satoh H, Miki A, et al. Medications associated with falls in older people: systematic review of publications from a recent 5-year period. Eur J Clin Pharmacol. 2015;71(12):1429-1440.
- Rojas-Fernandez C, Dadfar F, Wong A, et al. Use of fall risk increasing drugs in residents of retirement villages: a pilot study of long term care and retirement home residents in Ontario, Canada. BMC Res Notes. 2015;8:568.
- Ploughman M, Austin MW, Murdoch M, et al. The path to self-management: a qualitative study involving older people with multiple sclerosis. Physiother Can. 2012;64(1):6-17.