
Expired activity
Please go to the PowerPak
homepage and select a course.
Treatment of Narcolepsy Roused with New Mechanisms and Management Options: An Update for Pharmacists
Introduction
The term narcolepsy may evoke a simplistic image of a person falling asleep mid-sentence unexpectedly during the day because of a lack of adequate sleep. For years, narcolepsy was considered a single condition with therapies primarily centered on treating the symptoms (eg, daytime sleepiness, cataplexy), but the specifics of narcolepsy are more complex. As sleep research has advanced, two specific types of narcolepsy have been categorized: Narcolepsy Type 1 (NT1), which is characterized by excessive daytime sleepiness and cataplexy (a sudden loss in muscle tone often triggered by strong emotions); and Narcolepsy Type 2 (NT2), which is a more heterogeneous syndrome that includes the symptom of excessive sleepiness.1,2 Subsequently, researchers have elucidated components of the complex pathophysiology underlying the condition in which low levels of hypocretin (a neuropeptide previously known as orexin) play a dominant role in NT1, while the pathophysiology of NT2 remains unclear.1,2 With the evolution in the understanding of narcolepsy, new treatments have recently been approved that specifically target dysregulated sleep and wake pathways, and other therapies are on the horizon that target the pathophysiology of the condition rather than just the symptoms.
New Information About the Underlying Causes of Narcolepsy
Theories on the Pathophysiology of Narcolepsy
Case reports of narcolepsy were first published in western medical literature in the late 19th century that included descriptions of daytime sleepiness and cataplexy, symptoms that continue to be used in the diagnosis of the condition.3 With the gradual accumulation of research on the subject, defining points in the current understanding of narcolepsy include discoveries on the genetic component (via HLA DQB1*06-02) and the role of hypocretin in familial canine narcolepsy and human narcolepsy.2,3 These discoveries shaped the current understanding of narcolepsy and influenced ongoing drug discovery efforts. Essentially, persons with narcolepsy experience a lack of sleep regulation that results in very limited hours of sleep on the order of 1 to 3 hours. The lack of sleep regulation negatively impacts REM-stage sleep, which contributes to excessive daytime sleepiness and other symptoms such as hallucinations and cataplexy.2
Persons with NT1 have low levels of hypocretin and hypocretin cells such that a low level of hypocretin is one of the diagnostic criteria for NT1. The neuropeptide, hypocretin, activates the wake promoting centers in the brain.4 Hypocretin neurons are typically expressed in the hypothalamus and upward signaling to the locus coeruleus, substantia nigra, ventral tegmental area, raphe magnus, and tuberomammillary neurons facilitates wakefulness.5 In NT1, those neurons are irreversibly absent resulting in low or absent hypocretin levels.6 Consequently, the loss of wake-promoting signals from hypocretin and reductions in the signaling molecules norepinephrine, dopamine, and histamine leads to diminished or inconsistent transmission of the wake/arousal cycle. With the reductions in neurotransmitter signaling, drugs that increase the effects of histamine, norepinephrine, and dopamine have benefits in treating narcolepsy.
Researchers have discovered a number of hints to the mechanisms of the irreversible loss of hypothalamic hypocretin cells, including substantial indirect evidence for an autoimmune component driven by genetics.6,7 Genetics alone, however, do not fully explain the pathophysiology since there is a lack of concordance between monozygotic twins and the development of narcolepsy. On the other hand, since the concordance rate exceeds that associated with chance, there may be a gene or genes that impart susceptibility to narcolepsy.6,7 In fact, the presence of a specific allele, HLA-DQB1*06:02, of the human leukocyte antigen class II gene in persons with NT1 presents a major clue to an autoimmune origin and genetic component. That allele appears to be present in at least 92% of persons with NT1.8 Other evidence pointing toward an autoimmune component include an age of onset in adolescence/early adulthood and successful case reports using immune-based therapies.6 In addition, the autoimmune theory has been supported by observations in several European countries (but not the United States), where administration of a specific H1N1 vaccine, Pandemrix, appeared to be associated with a slightly increased risk for developing NT1. Carriers of the HLA-DQB1*06:02 allele exhibited an approximate 4-fold increase in risk of developing NT1.9 The proposed association between Pandemrix and narcolepsy is believed to involve cross-reactivity between the orexin 2 receptor and an influenza protein whose concentration is higher in Pandemrix compared to other H1N1 influenza vaccines.9
Diagnostic criteria: Narcolepsy Type 1 and Type 2
Narcolepsy is one of several central nervous system (CNS) disorders of hypersomnolence. With the 2014 update of the International Classification of Sleep Disorders (ICSD), the American Academy of Sleep Medicine changed the terminology describing narcolepsy to type 1 and type 2.10,11 The hallmarks of NT1 are low levels of hypocretin in the cerebrospinal fluid (CSF) or cataplexy confirmed by electrophysiology measurements. On the other hand, in NT2, normal CSF levels of hypocretin are observed or the lack of cataplexy is established through electrophysiology measurements.1,11 With the irreversible loss of hypocretin neurons in the hypothalamus, NT1 is considered a chronic condition. NT2 lacks a specific phenotype and persons with NT2 may see their symptoms dissipate or change in presentation to another hypersomnolence disorder.1
Delayed diagnosis of narcolepsy is common with some estimates on the order of 8 to 10 years or more.12,13 Onset of symptoms in childhood appears to be a major contributing factor to diagnostic delay.14 Avoiding diagnostic delay can limit the impact of misdiagnosis and lead to better health and psychosocial outcomes.13,15 Updated diagnostic criteria, particularly with hypocretin as a biomarker, have been developed with the ICSD 3rd edition. Diagnosis of NT1 requires the presence of 2 or more of the following criteria: cataplexy; multiple sleep latency tests (MSLT) with short sleep latency (< 8 min) and 2 or more sleep onset REM periods (SOREMPs); low levels of hypocretin in the CSF (≤ 110 pg/mL). NT2 relies more heavily on differential diagnosis including a history of excessive daytime sleepiness not explained by other causes; MSLT with short sleep latency (< 8 min) and 2 or more SOREMPs; absence of cataplexy; CSF hypocretin > 110 pg/mL or not measured.10 The diagnostic criteria for NT1 and type 2 are summarized in Table 1.
| Table 1. Diagnostic Criteria for Narcolepsy 1 and 2 |
| Narcolepsy 1 |
Narcolepsy 2 |
| History of EDS for at least 3 months |
History of EDS for at least 3 months (not explained by other causes) |
| Meets 2 or more of the following criteria: |
|
| Cataplexy |
No cataplexy |
Low CSF hypocretin
(≤ 110 pg/mL) |
CSF hypocretin > 110 pg/mL or not measured |
| MSLT with short sleep latency (average < 8 min) and 2 or more SOREMPs |
MSLT with short sleep latency (< 8 min) and 2 or more SOREMPs |
| EDS, excessive daytime sleepiness; SOREMP, sleep onset REM period; MSLT, multiple sleep latency tests |
Clinical Presentation
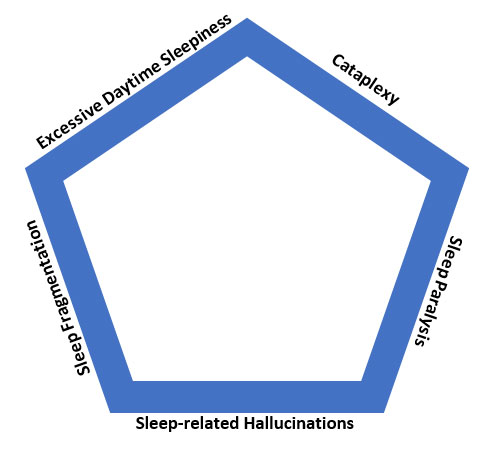
Increased awareness and understanding of narcolepsy symptoms are greatly needed as demonstrated by the AWAKEN survey as it identified substantial gaps in knowledge among the general population and clinicians (including sleep specialists).16 Diagnosis tends to peak in a bimodal pattern at approximately 15 years of age and 35 years of age.12 Persons with narcolepsy will typically present with symptoms in the narcolepsy pentad – excessive daytime sleepiness (EDS); cataplexy (for NT1); sleep fragmentation; sleep-related hallucinations; and sleep paralysis (see Figure 1).12,17 EDS, which the ICSD defines as “daily episodes of an irrepressible need to sleep or daytime lapses into sleep,” often presents during times of monotony or inactivity.1,18 In the course of disease onset, EDS symptoms may appear before REM manifestations. A person may wake up feeling alert, but episodes of EDS may ensue requiring naps that may recharge alertness for a period of time beyond which EDS recurs. Cataplexy, the sudden loss of muscle tone when experiencing strong emotions, can take the form of trembling knees, jaw dropping, head nodding, and falling to the ground.19 Cataplexy in children may present differently where presentation is often not connected to an emotion.11,17 The patients’ perspectives on cataplexy may also provide insights about triggering events. In narrative study of persons with NT1, recurrent themes focused on triggering situations (typically related to laughter), body sensations (particularly lack of strength in localized body areas), and management/control strategies (including avoiding or inhibiting strong emotions).20 Sleep fragmentation where multiple awakenings occur after the onset of sleep and recurrent shifts in sleep stages is a common symptom affecting upward of 90% of patients.21 Sleep-related hallucinations are vivid sensory events that occur during transitional states where hypnagogic hallucinations occur in the transition from wakefulness to sleep and hypnopompic hallucinations occur in the transition from sleep to wakefulness.1 As the term implies, sleep paralysis is a temporary loss (up to several minutes) of the ability to move during sleep transitions and may be accompanied by hallucinations.1
Figure 1. Narcolepsy Pentad
Prevalence and Burden of Disease
Narcolepsy is a relatively rare condition. The most recent prevalence data point to rates ranging from 0.02% to 0.18% for NT1 while the prevalence for NT2 is uncertain.17,22,23 Persons with narcolepsy can experience reduced quality of life in a number of domains: physical, psychological, social, family, and economic. Comorbidities with narcolepsy include mood disorders, anxiety, obesity, gastrointestinal diseases, hypercholesterolemia, hypertension, sleep apnea, metabolic disorder, and upper respiratory tract conditions.17,24 As result of the primary condition and the comorbidities, persons with narcolepsy tend to incur higher healthcare costs, earn less income, and use social services to a greater extent over their lifetimes compared to persons without narcolepsy.25,26 Greater disability, psychiatric comorbidity, work absenteeism, and healthcare utilization are also common for persons with narcolepsy.27 As an example of specific disease burden, the claims-based retrospective study by Black et al compared 9312 adults with narcolepsy with 46,559 matched adults without narcolepsy.26 The results showed approximately double the annual rate of several healthcare utilization parameters: inpatient admissions, emergency department visits without admission, hospital and other outpatient services, physician visits, and drug transactions (p < 0.0001 for each) in adults with narcolepsy compared to adults without.26 Costs for medical services and prescription drugs were also higher by at least two-fold in the narcolepsy group (medical costs: $8346 vs $4147, p < 0.0001; drug costs: $3356 vs $1114, p < 0.0001).26
As reviewed by Kallweit et al, several subjective tools are available to screen patients for narcolepsy or symptoms related to narcolepsy.19 The Ullanlinna Narcolepsy Scale is an 11-item inventory that assesses EDS and cataplexy to aid in distinguishing narcolepsy from other conditions. The Swiss Narcolepsy Scale is a 5-item tool that may be useful as a quick screening assessment. With 146 items and 9 sections, the Stanford Sleep Inventory can provide a more comprehensive assessment of symptoms in persons with narcolepsy although the length of the questionnaire may limit utility. The Cataplexy Emotional Trigger Questionnaire, a derivative of the Stanford Sleep Inventory, has been proposed to aid in distinguishing between cataplexy in narcolepsy vs cataplexy in other disorders. The Epworth Sleepiness Scale can be used as a measure of patient-reported EDS symptoms whether for narcolepsy or for other sleep disorders.19 At least two other questionnaires focus on assessment of symptoms that, if validated, may be useful for evaluating efficacy of narcolepsy treatments.19
For objective diagnosis of narcolepsy, the MSLT is used following an overnight sleep study (polysomnography). Overnight polysomnography rules out other potential underlying sleep disorders that could cause EDS.28 During the MSLT, individuals are instructed to attempt to fall asleep every 2 hours for five 20-minute nap periods (eg, 10 am, noon, 2 pm, 4 pm, and 6 pm).29 The individual then remains awake until the next nap period. A “positive” MSLT is characterized by a short sleep latency on naps (average < 8 min) and the appearance of REM sleep during 2 or more naps.
Overview of Narcolepsy Medications: Clinical Practice Guidelines
With no cure for narcolepsy, managing the condition focuses on treating the pentad of symptoms: EDS, sleep fragmentation, sleep-related hallucinations, sleep paralysis, and cataplexy. The American Academy of Sleep Medicine recently published updated clinical practice guidelines for the treatment of central disorders of hypersomnolence, including narcolepsy.30 The new clinical practice guidelines recommend medications for treatment of narcolepsy in adults with either a “strong” or “conditional” recommendation. The guidelines state that a recommendation of “strong” can also be interpreted as “we recommend” and should be followed by clinicians under most circumstances.30 A “conditional” recommendation can be interpreted as “we suggest” and leads to the clinician using clinical judgment, experience, and patient values and preferences to guide decision-making.30
Recommendations are made for treatment of narcolepsy, in general, with specific documentation of the clinical outcomes of narcolepsy improved by individual treatments. The clinical outcomes addressed include: excessive daytime sleepiness, cataplexy, disease severity, and quality of life.30 The clinical practice guidelines did not address medications based on categories (e.g. amphetamines, as a class), but rather on individual medications and the data supporting their use. The guideline states that prodrugs, enantiomers, different salts, and racemic compounds may have similar benefits and risks to the recommended therapies. A summary of the clinical practice guideline recommendations for medications used to treat adult narcolepsy is provided in Table 2.
| Table 2. Summary of Clinical Practice Guideline Recommendations for Treatment of Adult Narcolepsy30 |
| Medication |
Strength of Recommendation |
Outcomes Showing Clinically Significant Improvement |
| EDS |
Cataplexy |
Disease Severity |
Quality of Life |
| Modafinil |
Strong |
X |
X |
X |
|
| Pitolisant |
Strong |
X |
X |
X |
|
| Sodium Oxybate |
Strong |
X |
X |
X |
|
| Solriamfetol |
Strong |
X |
X |
X |
|
| Armodafinil |
Conditional |
X |
X |
| |
| Dextroamphetamine |
Conditional |
X |
X |
|
|
| Methylphenidate |
Conditional |
X |
|
|
|
| EDS = excessive daytime sleepiness |
Older Therapies
To treat EDS, traditional stimulant drug therapies include amphetamines and methylphenidate. Dextroamphetamine and methylphenidate are recommended (conditional) by the clinical guidelines. With the advent of newer pharmacotherapy agents, these drugs are considered second-line therapies.17,30 The stimulant drugs approved for narcolepsy, amphetamine (containing salts of amphetamine and dextroamphetamine) and methylphenidate, with their high potential for abuse and dependence, are Schedule II prescription products.31,32 Coupled with the high potential for abuse is the risk of tolerance and drug diversion.17 Extended-, intermediate-, or controlled-release formulations may mitigate the abuse/diversion potential and offer dosing flexibility to promote wakefulness over the desired wake period. In the use of stimulants for EDS in persons with narcolepsy, one should also consider the risk of adverse effects, particularly cardiovascular.17 The average adult dose for methylphenidate is 20 mg to 30 mg per day divided in 2 or 3 doses with a maximum daily dose of 60 mg.32 For amphetamines, the typical adult dose depends on individual response and varies from 5 mg to 60 mg per day (in divided doses).31
Traditional therapies for cataplexy, sleep paralysis, and other REM sleep abnormalities have included nonsedating tricyclic antidepressants, selective serotonin reuptake inhibitors (SSRIs), atomoxetine, and selective norepinephrine reuptake inhibitors (SNRIs) that suppress REM sleep. Although typically used for initial treatment based on cost and availability, none of these agents are FDA approved for treatment of cataplexy. The only FDA-approved treatments for cataplexy are limited to sodium oxybate, the low-sodium oxybate product, and pitolisant. Nonsedating tricyclic antidepressants, SSRIs, and SNRIs can be effective agents for treatment of cataplexy and work via enhanced aminergic signaling in the locus coeruleus and other CNS regions that regulate REM sleep. Despite having a limited number of clinical trials demonstrating effectiveness of these agents, they are routinely used as first-line agents in clinical practice due to low cost and relative effectiveness.
Nighttime sleep disruption is an underappreciated symptom of narcolepsy and has been poorly described and investigated. Patients with narcolepsy experience frequent nighttime awakenings and poor sleep quality. Although not specifically addressed by the new clinical practice guidelines, disturbed nocturnal sleep in narcolepsy has typically been managed with sodium oxybate and hypnotics. Clinically, benzodiazepines and nonbenzodiazepines (zolpidem, zaleplon, and eszopiclone) have been used to treat disrupted nighttime sleep but they have not been studied for that use. Sodium oxybate (described in detail below) has shown benefit in improving nighttime sleep.
Update on Targeted Therapies for Narcolepsy
Pitolisant – Pitolisant is the most recently FDA-approved agent with indications for both EDS and cataplexy in persons with narcolepsy and was given a “strong” recommendation by clinical practice guidelines.30,33 Pitolisant has a novel mechanism of action as an antagonist/inverse agonist of the histamine-3 receptor distinct from other narcolepsy pharmacotherapies.34 The suggested dosing of pitolisant is 17.8 mg to 35.6 mg once daily in the morning after following a dose titration schedule: 8.9 mg once a day for the first week of therapy, followed by 17.8 mg once a day in week two, and increasing to 35.6 mg if needed in week three and thereafter.33 With the absence of abuse potential, pitolisant has the advantage of not being a controlled substance, unlike many other narcolepsy drugs. Pitolisant, alone or in combination with other drugs, has shown efficacy in treating other symptoms in the narcolepsy pentad, ie, hallucinations and sleep paralysis.35 Its demonstrated effectiveness to additively enhance wakefulness when used with other medications is a unique aspect of pitolisant owing to its different mechanism of action. Primarily metabolized by CYP2D6 as well as CYP3A4, pitolisant may require dose adjustments if co-administered with strong CYP2D6 inhibitors or strong CYP3A4 inducers. Lower doses are recommended for poor CYP2D6 metabolizers, persons with moderate hepatic impairment, and persons with moderate-to-severe renal impairment. Pitolisant is not recommended for persons in end stage renal disease. As a CYP3A4 inducer, pitolisant may reduce the effectiveness of CYP3A4 substrates including hormonal contraceptives. Therefore, females of reproductive potential should be advised to use alternative, nonhormonal contraceptive methods during treatment with pitolisant and for ≥ 21 days after the last dose of pitolisant. In addition, the use of pitolisant may result in QT interval prolongation.33
Solriamfetol - Approved by the FDA in 2019 with the indication for improving wakefulness in adults with EDS from narcolepsy or obstructive sleep apnea, solriamfetol inhibits dopamine and norepinephrine transporters to prevent the reuptake of the neurotransmitters at the synapse.36,37 Solriamfetol was also given a “strong” recommendation for use by the clinical practice guidelines.30 In persons with narcolepsy, the starting dose of solriamfetol is 75 mg daily in the morning upon awakening and can be increased every 3 days up to a maximum of 150 mg. Dose adjustments are necessary in renal impairment. With moderate renal impairment (eGFR 30-59 mL/min/1.73 m2), the recommended starting dose is 37.5 mg once daily with a maximum of 75 once daily after a minimum of 7 days. Dosing in severe renal impairment (eGFR 15-29 mL/min/1.73 m2) is limited to 37.5 mg once daily while the drug is not recommended for persons in end stage renal disease.36 When treating obstructive sleep apnea, the starting dose of solriamfetol is 37.5 mg once daily. Of note, solriamfetol may increase blood pressure or heart rate and is contraindicated with monoamine oxidase inhibitors.36 In addition, solriamfetol is currently a Schedule IV controlled substance. Recent studies suggest that solriamfetol may normalize EDS (measured via Epworth Sleepiness Scale) compared to placebo38 and may also improve functional status, health-related quality of life, and work productivity.39 This data led the clinical practice guidelines to state that solriamfetol produces clinically significant improvements in quality of life.30
Modafinil/Armodafinil – Modafinil and armodafinil are indicated for promoting wakefulness in narcolepsy and other conditions but they do not have effects on cataplexy.40,41 Modafinil has a “strong” and armodafinil has a “conditional” recommendation according to the clinical practice guidelines,30 and are classified as Schedule IV controlled substances. In persons with narcolepsy, typical daily dosing for modafinil is 200 mg and for armodafinil is 150 mg to 250 mg administered in the morning.40,41 While the mechanisms of action of modafinil and armodafinil (the R-enantiomer of modafinil) are not entirely clear, the compounds appear to block dopamine reuptake by binding competitively to the dopamine transporter.42-44 The increase in dopamine along with increased transmission in adrenergic and histaminergic pathways combine to promote wakefulness.42,44 When used on a chronic basis, modafinil/armodafinil can induce CYP3A4, which can increase estrogen metabolism and reduce the effectiveness of hormonal contraceptives.40,41 Females of reproductive potential, therefore, should use alternative, nonhormonal contraceptive methods during treatment with modafinil/armodafinil and for ≥ 1 month after modafinil/armodafinil therapy is discontinued. Clinicians should be aware of a few important warnings and precautions associated with modafinil/armodafinil. Of note, modafinil/armodafinil are not approved for any indication in children. Hypersensitivity and allergic reactions have been reported that include serious rash, Stevens-Johnson Syndrome, angioedema, drug rash with eosinophilia and systemic symptoms, and multi-organ hypersensitivity reaction.40,41
Sodium Oxybate/Calcium/Potassium/Sodium Oxybates
Approved for the treatment of EDS and cataplexy in persons with narcolepsy who are ≥ 7 years old, the oxybates are salts of gamma-hydroxybutyrate (GHB).45,46 Practice guidelines give sodium oxybate a “strong” recommendation for treatment of narcolepsy. While the specific mechanism of action in narcolepsy is unknown, these CNS depressants increase daytime alertness by consolidating nighttime REM sleep and increasing slow-wave sleep. The effects may be the result of stimulating gamma aminobutyric acid B (GABAB) and its own GHB receptors. Outside of clinical practice, GHB is also a well-known drug of abuse and there is an associated risk of diversion/abuse with the prescription oxybate products. Both of the products, Xyrem (sodium oxybate) and Xywav (calcium/potassium/sodium oxybates) are available only through Risk Evaluation and Mitigation Strategy (REMS) programs and specialty pharmacies rather than through standard retail pharmacies.45–48 The high amount of sodium in Xyrem (820 mg/4.5 grams) (a potential concern in patients with hypertension, heart failure, and kidney disease) led to the development of the lower sodium product, Xywav, which consists of calcium, magnesium, potassium, and sodium salts of oxybate. Both products have the same adult dosage: an initial dose of 4.5 g per night in 2 divided doses then titrated to desired effect at a rate of 1.5 g per night per week up to 6 g to 9 g per night.45,46 The unique recommended dosing schedule specifies half of the dose to be taken at bedtime followed by the other half of the dose 2.5 to 4 hours later.45,46 The rapid onset of action of oxybates, where sleep generally ensues within 5 to 15 minutes after administration, necessitates special administration instructions as follows: prepare both doses before bedtime (ie, dilute each dose separately in 60 mL of water in child-resistant containers provided); take doses while in bed and lie down immediately after dose; take the first dose at least 2 hours after eating; an alarm may be needed to awaken patient for the second dose; never take both doses at one time.45,46 As CNS depressants, there is risk of respiratory depression and other CNS depressants such as alcohol and sedative hypnotics are contraindicated with the oxybates. An additional contraindication is succinic semialdehyde dehydrogenase deficiency.45,46
Investigational Categories
With the recent approvals of solriamfetol, pitolisant, and potassium/calcium/magnesium/sodium oxybate, practitioners have more therapeutic tools available to treat narcolepsy and improve patients’ lives. A summary of current drugs approved for treating narcolepsy symptoms is listed in Table 3. However, other therapies are on the horizon that complement current therapies and some that even specifically target hypocretin replacement. As the oxybate medications have a short duration of action, they require twice-nightly dosing, and resultantly, a long-acting sodium oxybate product is under development. Once-nightly dosing with similar effectiveness would be a therapeutic advancement allowing patients to sleep through the night without the need to awaken and re-dose. Reboxetine, a norepinephrine reuptake inhibitor that is approved in other countries, is also in development for the treatment of EDS and cataplexy. A phase II study is was begun in 2019 but no results are available yet. Additionally, research into the combination of modafinil and flecainide is also being pursued for narcolepsy. Flecainide works as an anticonnexin agent, which may enhance the effects of modafinil. Perhaps most importantly, hypocretin2 receptor agonists – (TAK-925 and TAK-994) are being developed and have shown promising results in preclinical studies49 and exploratory efficacy studies in patients with NT1.50 If effective, hypocretin replacement therapies represent the best chance to normalize the pathophysiologic abnormalities that occur due to loss of hypocretin neurons.
| Table 3. Overview of Medications Used to Treat EDS in Narcolepsy |
| Drug |
Indication(s) |
MOA |
Total Daily Dose |
Common Adverse Events |
Pharmacokinetics |
| Amphetamines |
EDS |
Inhibit NE and DA reuptake and enhance NE and DA release |
5-60 mg |
Insomnia, headache, decreased appetite, anxiety, modest increases in BP and HR |
Absorption is reduced when taken with acidic foods |
| Methylphenidate |
EDS |
Inhibit NE and DA reuptake |
5-60 mg |
Insomnia, headache, decreased appetite, anxiety, modest increases in BP and HR |
May increase bleeding risk in patients taking warfarin |
| Pitolisant |
EDS and cataplexy |
Histamine-3 receptor inverse agonist/
antagonist |
8.9-35.6 mg |
Headache, anxiety, insomnia, QT interval prolongation |
Possible CYP3A4 inducer – may render hormonal contraceptives less effective |
| Solriamfetol |
EDS |
Dopamine/norepinephrine reuptake inhibitor |
75-150 mg |
Headache, anxiety, insomnia, reduced appetite, modest increases in BP and HR |
Dose reductions required for impaired renal function |
| Modafinil |
EDS |
Increase DA by blocking DA transporters |
100-400 mg |
Headache, nausea, nervousness, rhinitis, diarrhea, back pain, anxiety, insomnia, dizziness, and dyspepsia |
CYP3A4 inducer – may render hormonal contraceptives less effective |
| Armodafinil |
EDS |
Increase DA by blocking DA transporters |
150-250 mg |
Headache, nausea, dizziness, and insomnia |
CYP3A4 inducer – may render hormonal contraceptives less effective |
Oxybates
(sodium, calcium, or potassium) |
EDS and cataplexy |
Stimulates GABA-B and GHB receptors |
4.5-9 g |
Nausea, headache, sweating, reduced appetite, anxiety, drowsiness, dizziness |
Rapid onset of action requiring administration while in bed in divided doses; Metabolized by tricarboxylic acid cycle to carbon dioxide and water |
Pharmacist's Role in Managing Narcolepsy
Rationale for pharmacotherapy of narcolepsy: Goals of pharmacotherapy for persons with narcolepsy focus on relieving the associated symptoms to improve functionality during the daytime and to increase quality of life. As described above, untreated narcolepsy contributes substantially to disability, comorbidities, lower quality of life, and increased direct and indirect costs.17,24–27 Effective treatments of narcolepsy symptoms are expected to produce improvements in the lives of persons with narcolepsy. Such improvements have been observed with sodium oxybate,51 modafinil,52 pitolisant,53 and solriamfetol.39 With the relative rarity of narcolepsy and potential for drugs that target the pathophysiology of narcolepsy, continuing research on pharmacotherapy effectiveness, including direct comparison of agents, is warranted. Pharmacists have medication expertise that can be applied for patients with narcolepsy to help them navigate side effects, drug interactions, and use with other comorbid conditions.
Managed care and specialty pharmacy issues: With the REMS programs required for the oxybate drug products and pitolisant restricted to select specialty pharmacies, specialty pharmacists can be directly involved in managing the treatment of persons with narcolepsy. Pharmacists from other practice areas may be involved by directing patients to the REMS and specialty pharmacy programs, whose pharmacists work with health insurance payors to determine/assist with obtaining coverage. In addition, pharmacists in managed care, ambulatory care, and community pharmacy can assist in helping payors understand the critical need for wake-promoting and other narcolepsy therapies as there is an increasing trend of traditional stimulants not being covered for EDS (narcolepsy and idiopathic hypersomnia). Upon such approval, a specialty pharmacy will send medication directly to the patient. The drug manufacturers may also provide some financial support options as well as patient education through their websites and associated patient advocacy/support groups.
Advising patients about dosage and administration: The various pharmacotherapy options for narcolepsy often require specific dosing regimens in order to enhance therapeutic outcomes while limiting any negative impact on nighttime sleep. Pharmacists can monitor and provide advice on maximum doses to optimize outcomes and minimize adverse events. Specific dosing instructions are common for the narcolepsy drugs. Amphetamines must not be administered with citrus or acidic foods with a 2-hour window between dosing and ingestion of such foods. The use of IR and SR formulations are often used in combination to cover the need for wakefulness during the day, which requires administering the SR formulation early in the day and the IR formulation later in the day during periods of required alertness (without carryover effects negatively influencing sleep). The oxybates have very specific dosing instructions (1 dose at bedtime followed by another dose 2.5 to 4 hours later) that are critical to emphasize in pharmacist consultations. Furthermore, combination therapies with drugs from different classes are common—particularly to address the different symptoms in the narcolepsy pentad, and pharmacists’ knowledge is essential to help patients safely and effectively implement appropriate combination therapies to optimize narcolepsy symptom control. For example, sodium oxybate, pitolisant, and modafinil may be used in combination with traditional stimulants, but they require careful management to enhance treatment success and minimize complications. There are listed drug-drug interactions between traditional cataplexy therapies (tricyclic antidepressants, SSRIs) and wake-promoting medications, but if correctly monitored and patients are educated to the risks by pharmacists, combination therapy can be safely pursued.
Advising patients about medication safety: Consistent with their typical responsibilities, pharmacists are the primary health care practitioner that has the knowledge, access, and context to screen for and educate patients regarding contraindications/cautions, drug-drug, and drug-disease interactions for narcolepsy therapies. Making patients aware of medication safety issues is a primary service that pharmacists provide. The two common safety concerns are contraindications with other medications and potential drug interactions. Many of these were discussed above for each individual drug (eg, reduction in hormonal contraceptive efficacy by modafinil/armodafinil and pitolisant; avoiding other CNS depressants with the oxybate formulations; potential for QT prolongation with pitolisant). Other potential safety issues include possible lowering of seizure threshold with amphetamines, methylphenidate, or modafinil/armodafinil. When considering amphetamines/methylphenidate, pharmacists can advise on IR and/or SR formulations to help reduce incidence of side effects associated with peak concentrations of the medication.
Adherence: As with other chronic conditions, improving medication adherence can help improve health outcomes. For narcolepsy drugs, there are some unique aspects in which pharmacist counseling can make a major difference in medication adherence.54 The second dose of the oxybate formulations (2.5 to 4 hours after bedtime) can be a challenge for many patients and pharmacists should counsel patients to set a recurring alarm on their clock or smartphone so that the second dose is not missed. For several of the narcolepsy drugs that treat EDS, timing the dose for the morning (often directly upon awakening) can help improve efficacy while avoiding symptoms of insomnia at bedtime. When available, SR formulations (such as those for amphetamines and methylphenidate) may be useful in boosting adherence and tolerability as the frequency of dosing is decreased. Pharmacists also may consider counseling patients about avoiding high amounts of caffeine while taking wake-promoting medications to clarify the medication benefits and reduce the risk of side effects.
Summary
Narcolepsy is a rare neurologic sleep disorder categorized into Type 1 (NT1) and Type 2 (NT2) forms—both of which share the symptom of excessive daytime sleepiness (EDS). Recent evidence suggests that the pathophysiology of NT1 centers on the loss of hypocretin neurons in the hypothalamus while the pathophysiology of NT2 is not fully understood. Narcolepsy has a significant disease burden on persons with the condition that include lower measures of health quality, a range of comorbidities, substantial increases in direct and indirect healthcare costs, and more. With no known cure for narcolepsy, pharmacotherapy primarily focuses on managing the symptoms of EDS and, for NT1, cataplexy. Newer drugs, such as pitolisant and solriamfetol, provide additional options for the management of narcolepsy. With a variety of mechanisms of action, combination therapies are often considered in order to treat EDS, cataplexy, and other symptoms of the narcolepsy pentad. Pharmacist involvement in the pharmacotherapy management of narcolepsy is critical given the distinctive characteristics of some of the available drugs including: REMS programs (for Xyrem and Xywav); unique dose administration schedules (particularly the oxybates); dose adjustments in renal insufficiency; availability of intermediate and/or extended release formulation; among others. With an understanding of the known pathophysiology and the available drugs, pharmacists can play active roles in the effective care of persons with narcolepsy.
References
- Dauvilliers Y, Barateau L. Narcolepsy and other central hypersomnias. Contin Lifelong Learn Neurol. 2017;23:989-1004. doi:10.1212/CON.0000000000000492.
- Reading PJ. Update on narcolepsy. J Neurol. 2019;266(7):1809-1815. doi:10.1007/s00415-019-09310-3.
- Mignot EJM. History of narcolepsy at Stanford University. Immunol Res. 2014;58(2-3):315-339. doi:10.1007/s12026-014-8513-4.
- Shi-Bin L, de Lecea L. The hypocretin (orexin) system: from a neural circuitry perspective. Neuropharmacology. 2020;167:107993. doi:10.1016/j.neuropharm.2020.107993.
- Peyron C, Tighe DK, Van Den Pol AN, et al. Neurons containing hypocretin (orexin) project to multiple neuronal systems. J Neurosci. 1998;18(23):9996-10015. doi:10.1523/jneurosci.18-23-09996.1998.
- Barateau L, Liblau R, Peyron C, Dauvilliers Y. Narcolepsy type 1 as an autoimmune disorder: evidence, and implications for pharmacological treatment. CNS Drugs. 2017;31(10):821-834. doi:10.1007/s40263-017-0464-6.
- Liblau RS, Vassalli A, Seifinejad A, Tafti M. Hypocretin (orexin) biology and the pathophysiology of narcolepsy with cataplexy. Lancet Neurol. 2015;14(3):318-328. doi:10.1016/S1474-4422(14)70218-2.
- Han F, Lin L, Schormair B, et al. HLA DQB1∗06:02 negative narcolepsy with hypocretin/orexin deficiency. Sleep. 2014;37(10):1601-1608. doi:10.5665/sleep.4066.
- Hallberg P, Smedje H, Eriksson N, et al. Pandemrix-induced narcolepsy is associated with genes related to immunity and neuronal survival. EBioMedicine. 2019;40:595-604. doi:10.1016/j.ebiom.2019.01.041.
- Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014;146(5):1387-1394. doi:10.1378/chest.14-0970.
- Thorpy M. International classification of sleep disorders. In: Chokroverty S, ed. Sleep Disorders Medicine: Basic Science, Technical Considerations and Clinical Aspects: Fourth Edition. 4th ed. New York: Springer New York; 2017:475-484. doi:10.1007/978-1-4939-6578-6_27.
- Morse AM. Narcolepsy in children and adults: a guide to improved recognition, diagnosis and management. Med Sci. 2019;7(12):106. doi:10.3390/medsci7120106.
- Thorpy MJ, Krieger AC. Delayed diagnosis of narcolepsy: characterization and impact. Sleep Med. 2014;15(5):502-507. doi:10.1016/j.sleep.2014.01.015.
- Maski K, Steinhart E, Williams D, et al. Listening to the patient voice in narcolepsy: diagnostic delay, disease burden, and treatment efficacy. J Clin Sleep Med. 2017;13(3):419-425. doi:10.5664/jcsm.6494.
- Thorpy MJ, Hiller G. The medical and economic burden of narcolepsy: implications for managed care - PubMed. Am Heal Drug Benefits. 2017;10(5):233-241.
- Rosenberg R, Kim AY. The AWAKEN survey: knowledge of narcolepsy among physicians and the general population. Postgrad Med. 2014;126(1):78-86. doi:10.3810/pgm.2014.01.2727.
- Abad VC, Guilleminault C. New developments in the management of narcolepsy. Nat Sci Sleep. 2017;9:39-57. doi:10.2147/NSS.S103467.
- Sleep Foundation. Narcolepsy. https://www.sleepfoundation.org/narcolepsy. Published 2021. Accessed May 16, 2021.
- Kallweit U, Schmidt M, Bassetti CL. Patient-reported measures of narcolepsy: The need for better assessment. J Clin Sleep Med. 2017;13(5):737-744. doi:10.5664/jcsm.6596.
- Franceschini C, Fante C, Folli MC, et al. Giving a voice to cataplectic experience: Recollections from patients with narcolepsy type 1. J Clin Sleep Med. 2020;16(4):597-603. doi:10.5664/jcsm.8286.
- Thorpy MJ. Update on therapy for narcolepsy. Curr Treat Options Neurol. 2015;17(5):347. doi:10.1007/s11940-015-0347-4.
- Iranzo A. Sleep and neurological autoimmune diseases. Neuropsychopharmacology. 2020;45(1):129-140. doi:10.1038/s41386-019-0463-z.
- Bassetti CLA, Adamantidis A, Burdakov D, et al. Narcolepsy — clinical spectrum, aetiopathophysiology, diagnosis and treatment. Nat Rev Neurol. 2019;15(9):519-539. doi:10.1038/s41582-019-0226-9.
- Kornum BR, Knudsen S, Ollila HM, et al. Narcolepsy. Nat Rev Dis Prim. 2017;3:16100. doi:10.1038/nrdp.2016.100.
- Jennum P, Ibsen R, Petersen ER, Knudsen S, Kjellberg J. Health, social, and economic consequences of narcolepsy: A controlled national study evaluating the societal effect on patients and their partners. Sleep Med. 2012;13(8):1086-1093. doi:10.1016/j.sleep.2012.06.006.
- Black J, Reaven NL, Funk SE, et al. The burden of narcolepsy disease (BOND) study: health-care utilization and cost findings. Sleep Med. 2014;15(5):522-529. doi:10.1016/j.sleep.2014.02.001.
- Flores NM, Villa KF, Black J, Chervin RD, Witt EA. The humanistic and economic burden of narcolepsy. J Clin Sleep Med. 2016;12(3):401-407. doi:10.5664/jcsm.5594.
- Carskadon MA, Dement WC, Mitler MM, Roth T, Westbrook PR, Keenan S. Guidelines for the multiple sleep latency test (MSLT): A standard measure of sleepiness. Sleep. 1987;9(4):519-524. doi:10.1093/sleep/9.4.519.
- Cao MT, Guilleminault C. Narcolepsy: diagnosis and management. In: Kryger MH, Roth T, Dement WC, eds. Principles and Practice of Sleep Medicine. 6th ed. Philadelphia, PA: Elsevier; 2017:873-882.
- Maski K, Trotti LM, Kotagal S, et al. Treatment of central disorders of hypersomnolence: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2021; https://doi.org/10.5664/jcsm.9328.
- Adderall [package insert]. Horsham, PA: Teva Pharmaceuticals USA; 2017.
- Ritalin [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2019.
- Pitolisant [package insert]. Plymouth Meeting, PA: Harmony Biosciences LLC; 2021.
- de Biase S, Pellitteri G, Gigli GL, Valente M. Evaluating pitolisant as a narcolepsy treatment option. Expert Opin Pharmacother. 2021;22(2):155-162. doi:10.1080/14656566.2020.1817387.
- Dauvilliers Y, Arnulf I, Szakacs Z, et al. Long-term use of pitolisant to treat patients with narcolepsy: Harmony III Study. Sleep. 2019;42(11). doi:10.1093/sleep/zsz174.
- Solriamfetol [package insert]. Palo Alto, CA: Jazz Pharmaceuticals; 2019.
- Powell J, Piszczatoski C, Garland S. Solriamfetol for excessive sleepiness in narcolepsy and obstructive sleep apnea. Ann Pharmacother. 2020;54(10):1016-1020. doi:10.1177/1060028020915537.
- Rosenberg R, Baladi M, Bron M. Clinically relevant effects of solriamfetol on excessive daytime sleepiness: a post hoc analysis of the magnitude of change in clinical trials in adults with narcolepsy or obstructive sleep apnea. J Clin Sleep Med. 2021;17(4). doi:10.5664/jcsm.9006.
- Emsellem HA, Thorpy MJ, Lammers GJ, et al. Measures of functional outcomes, work productivity, and quality of life from a randomized, phase 3 study of solriamfetol in participants with narcolepsy. Sleep Med. 2020;67:128-136. doi:10.1016/j.sleep.2019.11.1250.
- Modafinil [package insert]. North Wales, PA: Teva Pharmaceuticals USA; 2015.
- Armodafinil [package insert]. North Wales, PA: Teva Pharmaceuticals USA; 2018.
- Wisor J. Modafinil as a catecholaminergic agent: empirical evidence and unanswered questions. Front Neurol. 2013;4:139. doi:10.3389/fneur.2013.00139.
- Loland CJ, Mereu M, Okunola OM, et al. R-modafinil (armodafinil): A unique dopamine uptake inhibitor and potential medication for psychostimulant abuse. Biol Psychiatry. 2012;72(5):405-413. doi:10.1016/j.biopsych.2012.03.022.
- Wisor JP, Eriksson KS. Dopaminergic-adrenergic interactions in the wake promoting mechanism of modafinil. Neuroscience. 2005;132(4):1027-1034. doi:10.1016/j.neuroscience.2005.02.003.
- Xrem [package insert]. Palo Alto, CA: Jazz Pharmaceuticals; 2020.
- Xwav [package insert]. Palo Alto, CA: Jazz Pharmaceuticals; 2020.
- Jazz Pharmaceuticals. The XYWAV and XYREM REMS: an overview. https://www.xyremhcp.com/xywav-xyrem-rems. Published 2021. Accessed May 16, 2021.
- Strunc MJ, Black J, Lillaney P, et al. The Xyrem® (Sodium Oxybate) Risk Evaluation and Mitigation Strategy (REMS) Program in the USA: Results From 2016 to 2017. Drugs - Real World Outcomes. 2021;8(1):15-28. doi:10.1007/s40801-020-00223-6.
- Yukitake H, Fujimoto T, Ishikawa T, et al. TAK-925, an orexin 2 receptor-selective agonist, shows robust wake-promoting effects in mice. Pharmacol Biochem Behav. 2019;187:172794. doi:10.1016/j.pbb.2019.172794.
- Evans R, Tanaka S, Tanaka S, et al. A phase 1 single ascending dose study of a novel orexin 2 receptor agonist, TAK-925, in healthy volunteers (HV) and subjects with narcolepsy type 1 (NT1) to assess safety, tolerability, pharmacokinetics, and pharmacodynamic outcomes. Sleep Med. 2019;64(suppl 1):S105-S106. doi:10.1016/j.sleep.2019.11.290.
- Bogan R, Swick T, Mamelak M, et al. Evaluation of quality of life in patients with narcolepsy treated with sodium oxybate: use of the 36-item short-form health survey in a clinical trial. Neurol Ther. 2016;5(2):203-213. doi:10.1007/s40120-016-0053-5.
- Golicki D, Bala MM, Niewada M, Wierzbicka A. Modafinil for narcolepsy: systematic review and meta-analysis - PubMed. Med Sci Monit. 2010;16(8):RA177-RA186.
- Wang J, Li X, Yang S, et al. Pitolisant versus placebo for excessive daytime sleepiness in narcolepsy and obstructive sleep apnea: A meta-analysis from randomized controlled trials. Pharmacol Res. 2021;167:105522. doi:10.1016/j.phrs.2021.105522.
- Begley KJ, Castillo S, Steinshouer CR, Malesker MA. Role of pharmacists in the treatment of excessive daytime sleepiness. Consult Pharm. 2014;29(11):741-752. doi:10.4140/TCP.n.2014.741.
Back to Top