
Expired activity
Please go to the PowerPak
homepage and select a course.
Taking the Pulse of Undiagnosed Atrial Fibrillation: Pharmacists as a Lynchpin of Detection and Team-Based Care
Slide 1
Dr. Bleske: Hello. This is Barry Bleske from the University of New Mexico. Welcome to this educational activity focusing on taking multidisciplinary and novel approaches to detecting atrial fibrillation (AF) in the community setting. Joining me in today's discussion are Joe Anderson and Abinash Achrekar, who are also from the University of New Mexico.
Assessing the Burden of Undiagnosed AF: A Review of the Prevalence, Challenges, and Consequences
Slide 2
Dr. Bleske: So, let's begin. Dr. Achrekar, tell us a little bit about what AF is, and why are we here today talking about AF?
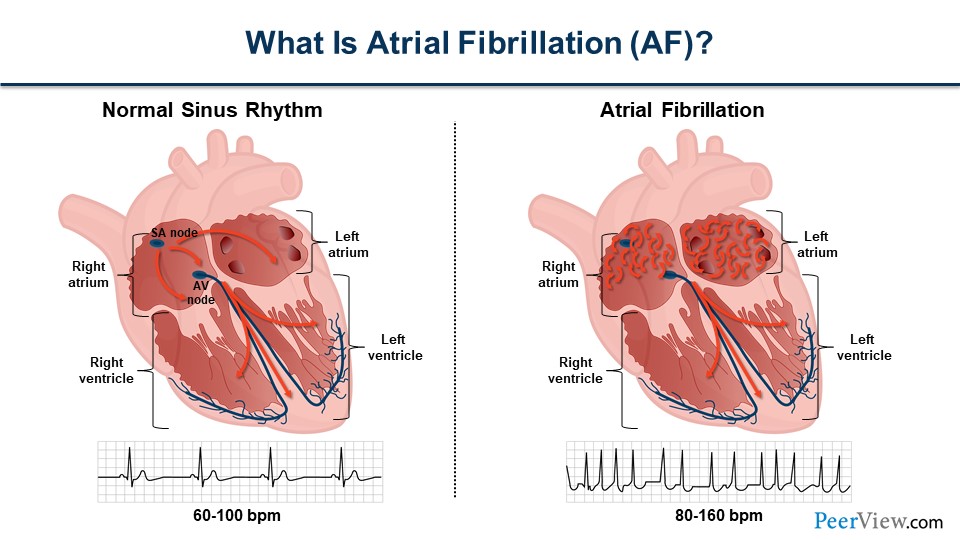
Dr. Achrekar: Thanks, Barry. A little bit about AF. So, AF is an abnormal heart rhythm. What we see on the left side of the figure is normal sinus rhythm. Electricity is generated in the top part of the heart called the atrium, and the right atrium, and it proceeds down through the His bundle that is kind of in the middle there. The ventricles, the big pumping chambers of the heart, then contract, and you can see what it looks like on an ECG below the illustration.
But AF, it's a different beast. It's a very common arrhythmia, and we'll talk about some of the risk factors later. But it's a chaotic and disorganized atrial electricity, as shown on the right side of the figure. Some of that electricity gets into that His bundle, and then the ventricles subsequently contract, but they contract in an irregular fashion. You can see how that's represented in ECG below that illustration.
Slide 3
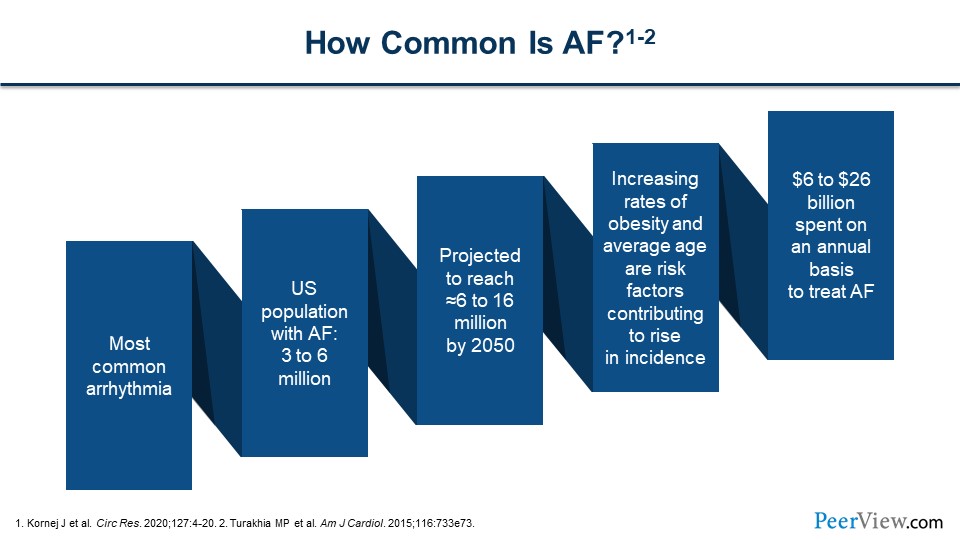
So, how common is AF? It's, very common. In fact, I've actually had AF myself, many years ago when I was in medical school. But it is a problem of aging. In the United States, at least 3 to 6 million people have AF, and as we have an aging population, that number is going to increase to 6 to 16 million by the year 2050.
Slide 4
Increased rates of obesity and the increasing average age are risk factors, as well as hypertension. This costs an immense amount of money per year—$6 to $26 billion to treat it annually.
Dr. Bleske: So one of the goals of this activity is to identify the ways in which pharmacists can work collaboratively with other clinical colleagues to really bridge the gap between patients and healthcare professionals to improve AF screening, diagnosis, and treatment. But Ash, why is it so important that we identify individuals with AF?
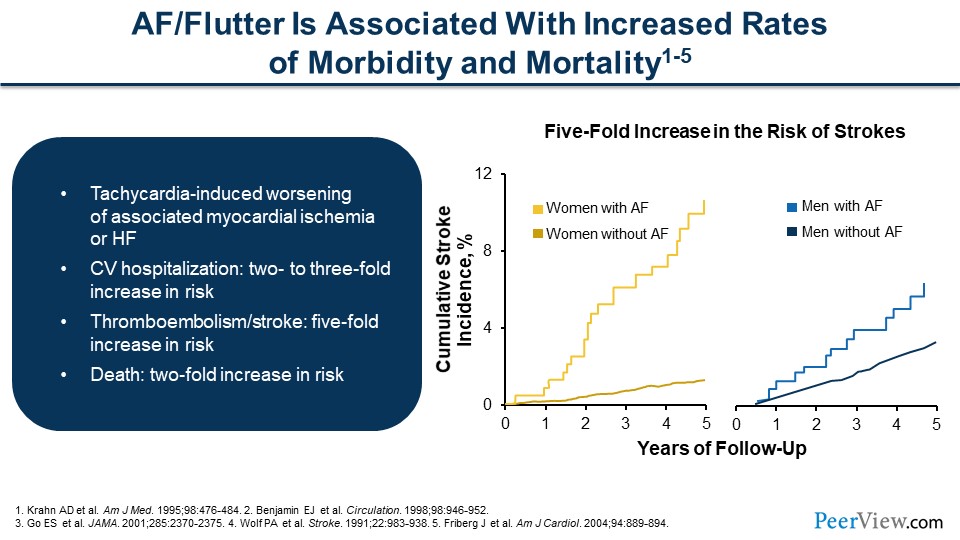
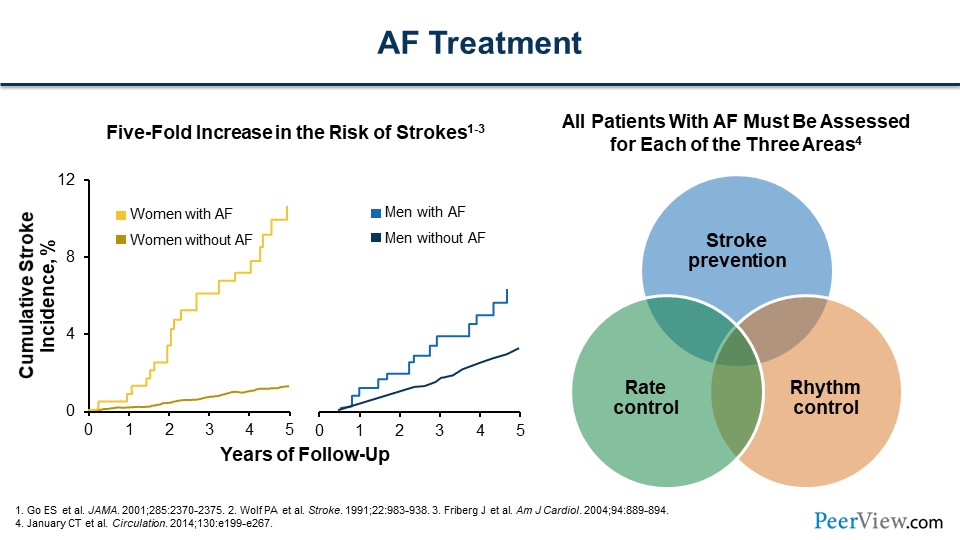
Dr. Achrekar: So, AF or flutter—it's a similar rhythm, it's generated a little bit differently, but the risk factors are the same—is associated with increased rates of morbidity and mortality. These rhythms, AF, can cause tachycardia, a fast heart rate, and that can be associated with ischemia, which is not enough blood flow to the heart muscle, and even heart failure (HF), a weakening of the heart muscle and developing symptoms. Cardiovascular (CV) hospitalization increases two- to threefold. Thromboembolism or stroke increases fivefold, depending on the risk factors, which we'll talk about later. But death increases as well, there’s a twofold increase in death. If we look at this figure, women are represented in yellow and men are on the right in blue. There is an increased cumulative stroke risk in women compared with men, and this is also delineated when we talk about a scoring for AF and the risk of stroke and systemic embolism (SE).
Slide 5
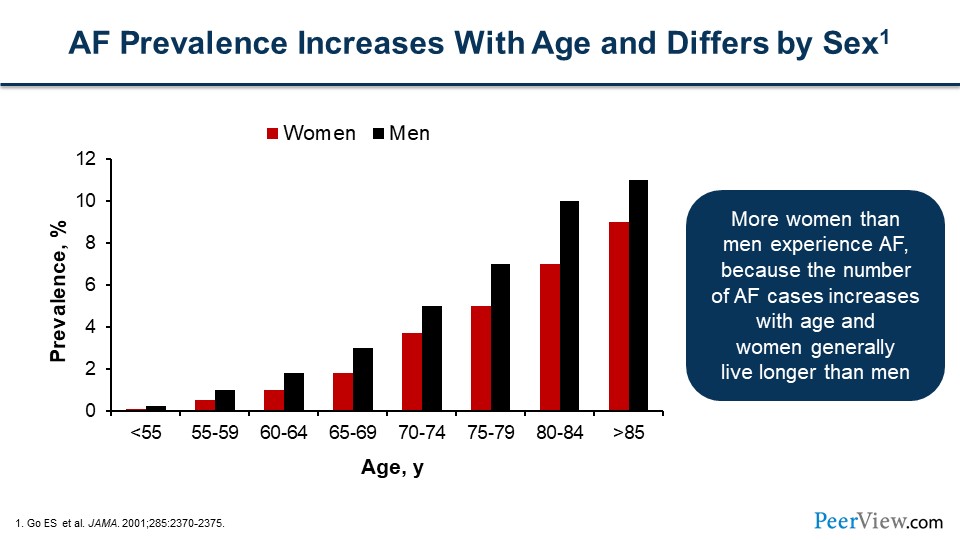
So, AF prevalence increases with age, and as we have an aging population, we're seeing more AF. I did say that there's more stroke in women than men, but there's actually more men than women who have stroke. In this figure, the black bars represent men and the red bars represent women. But as we know, women live longer than men, and so over time, there is more accumulation of women who have the burden of living with AF than men.
Slide 6
Dr. Bleske: With such a significant risk in stroke, it seems that it would be very important to prevent and detect AF. Ash, what are potentially some of the risk factors and symptoms associated with AF?
Dr. Achrekar: Thanks for the question, Barry. There are risk factors that have been really well defined from research models and historically, and there are some that are nonmodifiable, like age. We can't change your age, but there are modifiable risk factors that lead to the development of AF, as well as controlling some of the risks. Hypertension and high blood pressure (BP) for example. Heart disease is a modifiable risk factor that can be treated, as well as HF, hyperthyroidism, excessive alcohol intake, obesity, and sleep apnea. Add diabetes to this as well; it’s a modifiable risk factor that can be treated.
Slide 7
If we're talking about symptoms in general patients, what are they feeling? The interesting thing about AF is you can feel a lot of things. You can feel palpitations, which is a kind of a fluttering or an accelerated or irregular heartbeat. You can have fatigue if your heart rate is fast or irregular, which could represent tiredness. You can faint. Usually, this doesn't happen, but it can happen in an elderly patient or those who have a corresponding significant heart disease. They can sometimes syncopize or faint. You can have dyspnea, or shortness of breath, at rest or with physical activity. Sometimes lightheadedness as well; it is pretty common. And then, in those patients who have coronary artery disease, they may not have good coronary perfusion during times of rapid tachycardia in AF and can actually have angina as well.
Slide 8
But many patients are asymptomatic. I began saying I had AF when I was in medical school, but I went hours and hours, probably a half a day, in AF, not feeling it at all. That's not very uncommon. AF can have a triad of symptoms that include racing, fluttering heart palpitations, shortness of breath, and some lightheadedness or dizziness. But individuals can have no symptoms at all. There are some data to show that those in AF only know about half the time that they're in AF. So, you can't really ask a patient, "Do you feel it? Do you feel these palpitations?" If they say “no,” that doesn't necessarily mean they don't have AF.
Dr. Bleske: I think this is extremely important, because obviously if a patient comes to clinic or to the pharmacy short of breath or dizzy, it could be due to AF. But, as I was going to ask: What about the patients without symptoms? We know people with symptoms are at risk for stroke and potential death, but what about these asymptomatic patients?
Slide 9
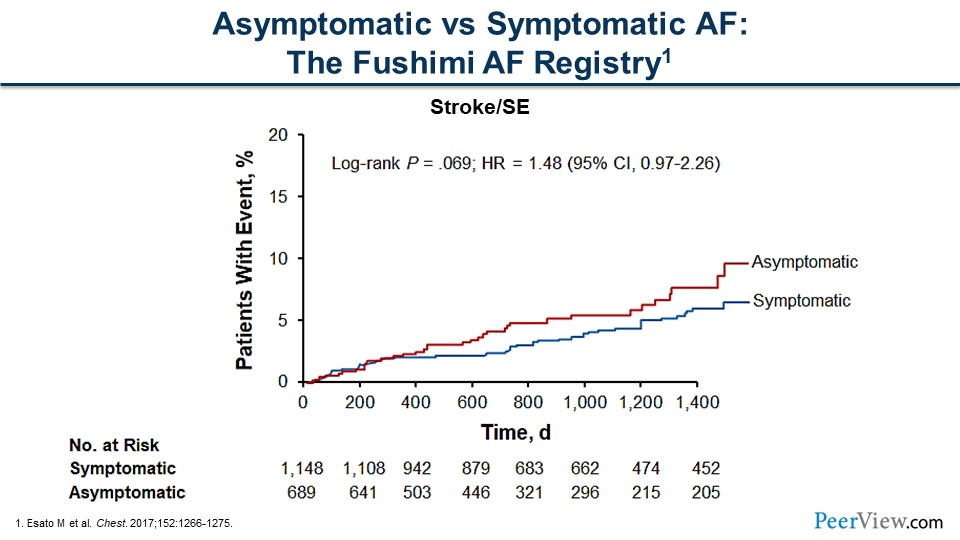
Dr. Achrekar: That's a great question. It's really difficult to treat a patient who doesn't feel bad. Many patients say, "I don't feel my AF. I don't need to worry about it." But this is figure shows symptomatic versus asymptomatic patients. The asymptomatic patients are represented in red, and patients with events are measured by the y-axis. There's actually a numerically higher increase in patients with events who are asymptomatic versus symptomatic. We should note that there's really no difference statistically between these two lines, and that tells us whether patients are symptomatic or asymptomatic, they are still at risk of having CV events, stroke, or SE.
Slide 10
Dr. Bleske: Yikes! That’s really not good news. Joe, how common is this asymptomatic or undetected AF?
Dr. Anderson: Thanks, Barry. As Ash mentioned, the risk of stroke in asymptomatic and symptomatic patients is about the same. A lot of recent research is focused on trying to identify the rates of silent or asymptomatic AF. Estimates vary. However, in general, from single-time-point screening in patients who are aged 65 years or older, undiagnosed AF is about 1.4%. More intensive screening programs, such as screening twice a day over a 2-week period, show the incidence is slightly higher, around 3%.
Slide 11
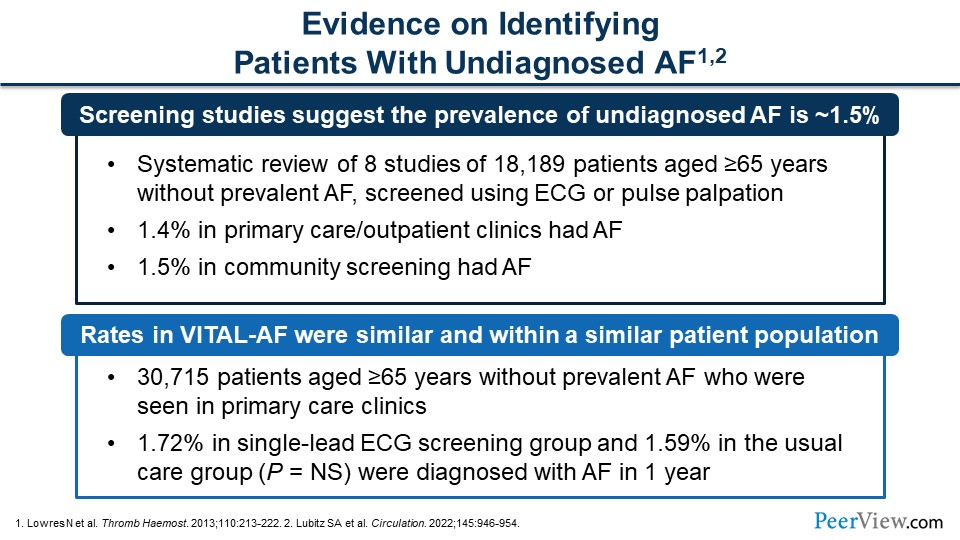
Dr. Anderson: And I note, our recent experience with both our opportunistic screenings at our student-driven health fairs and systematic screenings in community pharmacy settings, we're on the higher end. This might be reflective of a higher-risk population. I would like to add that a recent study called the VITAL-AF was just recently published in a similar population, patients over the age of 65 years but seen in a primary care clinic. They utilized a single-lead ECG screening or just usual care and found the incidence of asymptomatic AF in the screening group to be about 1.7%, which is very consistent with previous studies, versus 1.6% in usual care group—usual care consisting of pulse palpation or auscultation.
Slide 12
Dr. Bleske: This asymptomatic or undetected AF seems to be pretty important in managing AF, and it seems like we could be missing a lot of patients and diagnosing them with AF, if they have no symptoms. How do we identify or catch these patients?
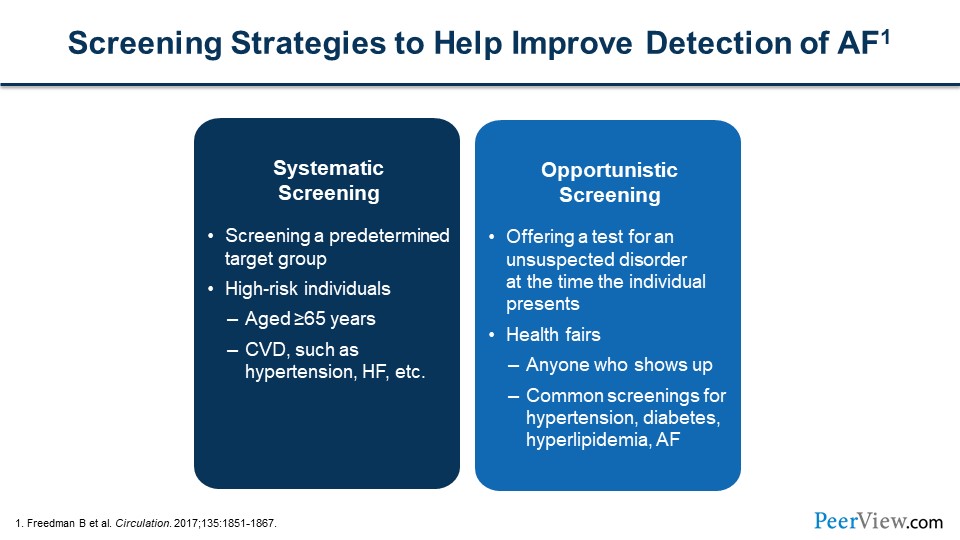
Dr. Anderson: That's the big question: How do we identify these individuals? You could do one of two methods. You can take a systematic approach to screening or an opportunistic approach to screening. In a systematic approach, you're taking a more targeted group, a higher-risk population, and then screening those individuals. Those studies that I mentioned, for example, chose individuals who were over the age of 65 years. As Ash mentioned, the risk of AF goes up with age. You could target individuals with risk factors for HF, such as hypertension, HF, diabetes, etc. So, an opportunistic screening would be more like a health fair, where you screen all-comers, regardless of risk. At that point in time, you're hopefully combining it with additional screening for risk factors, such as high BP, diabetes, etc.
Slide 13
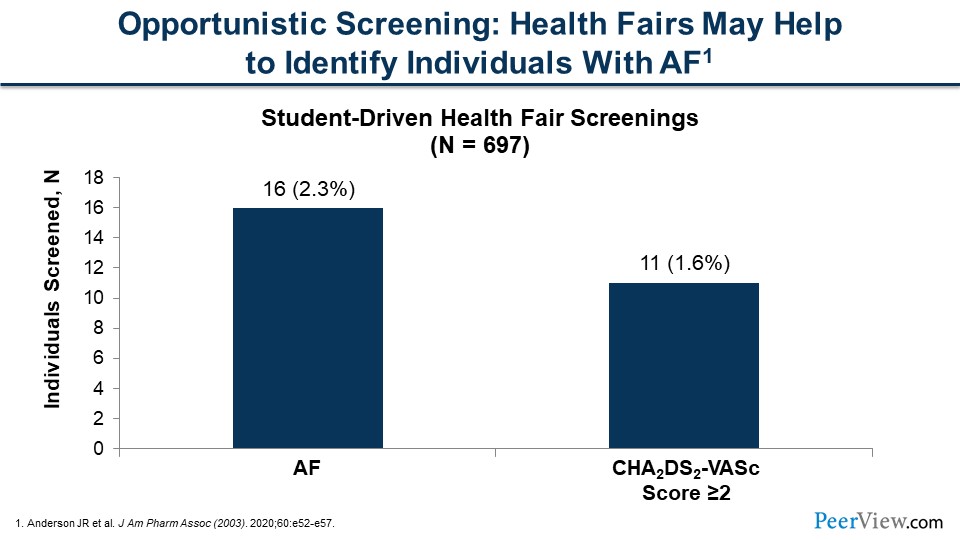
Dr. Anderson: This figure is an example that I alluded to earlier with an opportunistic screening that we've conducted at health fairs around our community. We found in the general population that came to the screening about a 2.3% incidence of AF detected with our single-lead ECG screening device. Looking at the higher-risk patients, we saw that the majority of these patients who were screened positive did have higher risk factors for stroke and that's important. That was why we were doing the screenings, because these are the individuals who are at higher risk for stroke.
Slide 14
As you know, in the old days screening was not easily conducted. If you were at a medical office, you had to have a 12-lead ECG and in patients with pulse palpation or auscultation who were determined to possibly have AF, you would have to have a 12-lead ECG in the office, perform that or send them off to perhaps a hospital or another provider for the 12-lead ECG screening. Or for those individuals who you might suspect have paroxysmal AF, you might have to hook them up to a Holter monitor for 24 or 48 hours.
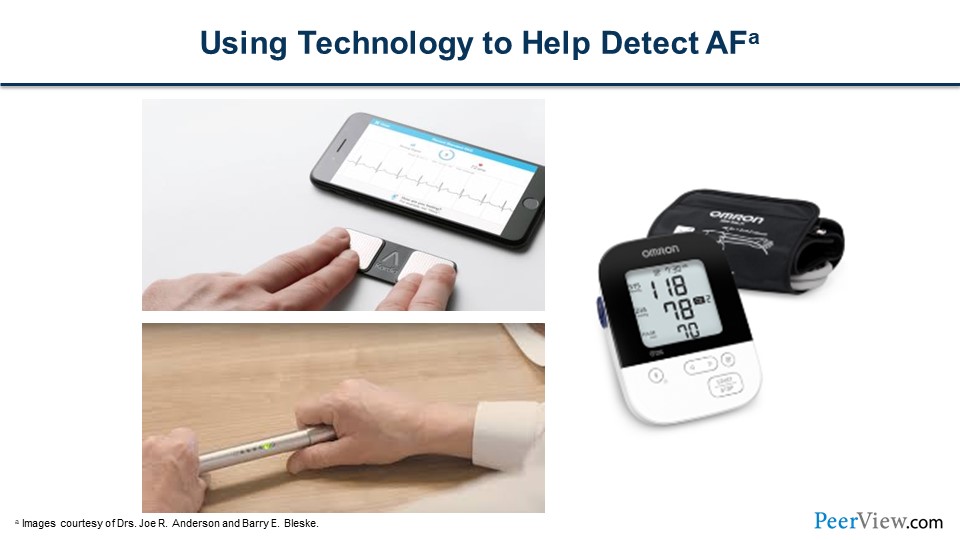
Slide 15
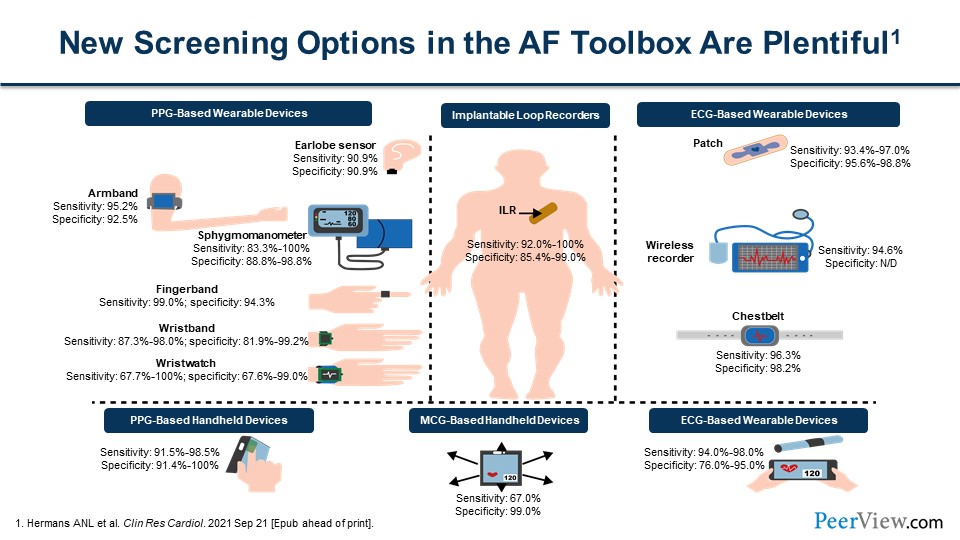
But with advances in technology, screening has become easier and much more efficient. We have a multitude of devices now that can be used for screening. Many people are familiar with the smartwatches that can be worn and used to screen for AF. There are advertisements on TV for devices that individuals can purchase and use to screen themselves for ECGs. These various devices have differences in sensitivity and specificity for picking up AF.
Ash, is there anything that you think needs to be added here with regard to these various devices in terms of sensitivity and specificity?
Slide 16
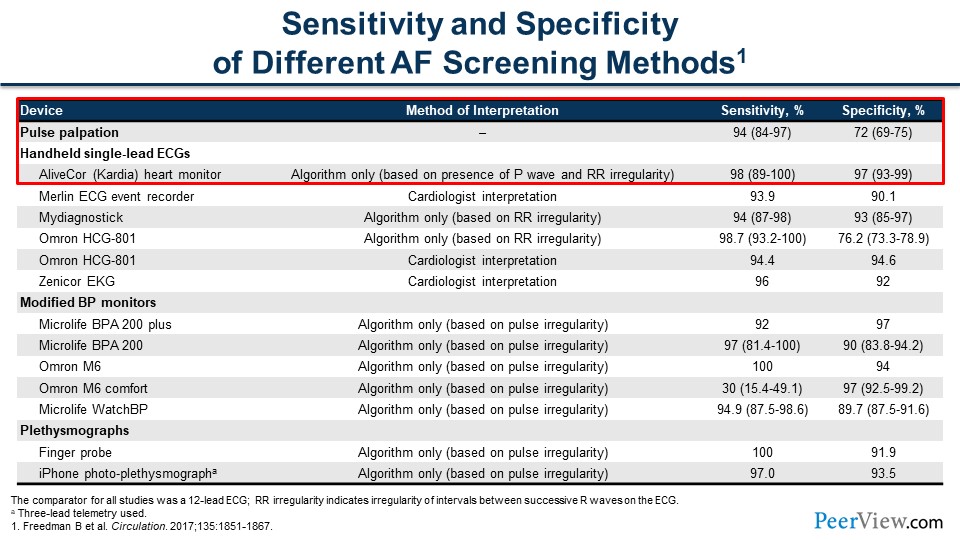
Dr. Achrekar: Joe, thanks for your question. This is really important. As we've seen in the previous slides, there are new advances in how we can detect AF. It started with just palpating a pulse to auscultating with a stethoscope to these really cumbersome monitors that we could either do a point-of-time ECG, which is just about 5 to 10 seconds of time, or these bulky Holter monitors that we would have people wear for a day or two.
As shown, there are many kinds of monitors, but the ideal method of screening has really high sensitivity, as well as really high specificity. If you look at pulse palpation, for example, there's a 94% sensitivity. This tells you that it's really good at ruling out if a patient doesn’t have AF, but its specificity is only about 72%. It's really not great at ruling it in. That's because people mostly have paroxysmal AF and they're not always in it. But if you look at some of the other devices, such as the AliveCor Kardia heart monitor, the specificity and sensitivity are much higher. As shown in the table down the columns, we've really improved with specificity and sensitivity. I think that's why it's probably a better way to start looking for AF in our community.
Slide 17
Dr. Anderson: Thank you, Ash. Technology is certainly amazing, but Barry, is it reasonable to screen and are there guidelines in regard to population screening for asymptomatic or undetected AF?
Slide 18
Dr. Bleske: When we think about population screening, we have to always balance risk to benefit and also feasibility. For screening to be enabled to screen a population, it needs to be inexpensive, easy to use, and have a high positive predictive value. Today, looking to screen for AF with the devices available and with the new technology, it really meets this criteria. It's less than $200. You can have the device. It's easy to use. Within 30 seconds, anyone can do it. As pointed out, it works pretty well in detecting AF, so from that standpoint, either opportunistic or systematic screening is very much feasible.
Are there positive outcomes? As Ash mentioned earlier, you have AF and you have risk factors. You're at high risk for stroke. Importantly and luckily, we have very efficient and very good pharmacotherapeutic options, such as anticoagulants, that can reduce stroke risk and mortality. From that positive outcome aspect, it is certainly something we want to consider, to screen on a population basis. As with anything, there are always negative aspects to consider. But you always want to consider are these acceptable outcomes? There is a cost; it's not free. There's time involved. You could potentially increase patient stress, office visits, overdiagnosis, the potential for unnecessary diagnosis, diagnostic testing, and treatment. Also, we don't yet have outcome data to show improved outcomes with population screening.
Slide 19
Dr. Bleske: Now, if we look at the guidelines, and we look at the guidelines in the United States from the US Preventive Service Task Force (USPSTF), they state that the current evidence is insufficient to assess the balance of benefits and harms of screening AF. But also in the guidelines, they also mention that we still need to consider pulse palpation to be part of routine or usual care. A couple of things to note: In the review by the USPSTF, it has to be noted that no eligible studies were found that evaluated harm in screening patients for AF as compared with no screening. Importantly, as I mentioned earlier, we have no outcome data. Joe has already talked about VITAL-AF and the similar detection rate with two different types of usual care versus single-lead ECG. But of note, in the usual care group, they did include automated devices, palpation, and auscultation as detection devices.
Looking at other guidelines from around the world, the European Society of Cardiology (ESC) does recommend opportunistic AF screening by pulse assessment or by ECG rhythm strip in patients aged 65 years or older. Guidelines also note that good settings for AF screening include pharmacies and community screening at special events. Looking at the Australian Heart Foundation, they have a similar sort of recommendation: Opportunistic point-of-care screening in the clinic or community setting should be conducted in people aged 65 years or older.
The Act of Unburdening: Harnessing the Untapped Resource of Pharmacists to Reduce Stroke Risk in NVAF
Slide 20
As mentioned, patients with AF may have significant risk for stroke. Stroke could be prevented with anticoagulant therapy. Joe, how can we find these patients who may be asymptomatic and walking around with AF but don't know they have it in a sustainable and, importantly, affordable approach?
Dr. Anderson: Thanks, Barry. That's a huge question. I would like to think that pharmacists are an answer and a pharmacist's role in this process depends on their location. Pharmacists who are in the community are an excellent resource. They're everywhere. They're in rural, urban, underserved areas. It's said that 90% of our population lives within 5 miles of a community pharmacy, so we're accessible. The community pharmacists could be a source for screening, using the devices that we've mentioned, through opportunistic or even systematic screenings and target a higher-risk patient population for screening.
Pharmacists in the clinic setting working with other healthcare providers can be utilized to screen but also to manage risk factors, so hopefully preventing the development of AF by better control of those risk factors. And then, once a patient does develop AF and requires anticoagulation, pharmacists are uniquely suited to run the anticoagulation clinics and control the levels of anticoagulation and avoid dangerous drug–drug interactions, as well as other interactions, with those agents.
Slide 21
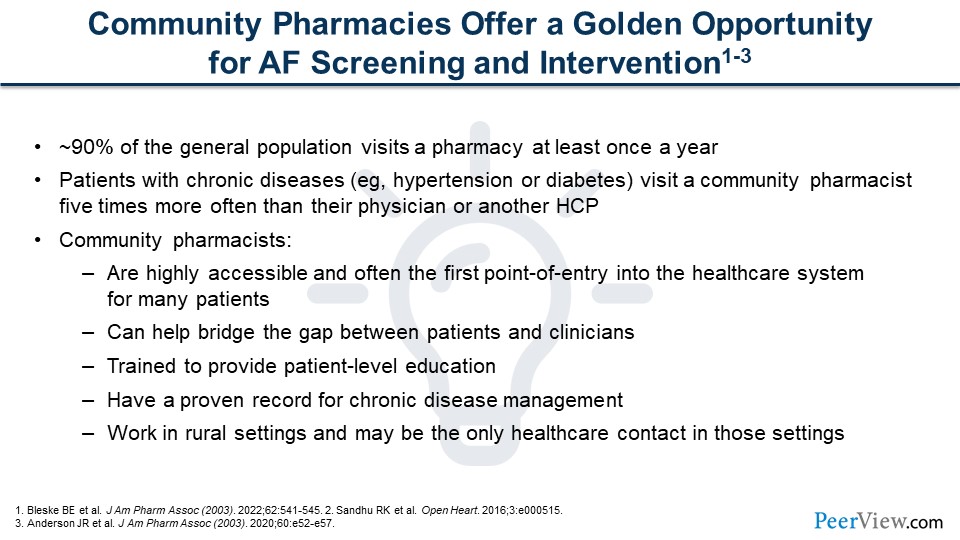
We really believe that community pharmacies offer a golden opportunity, and they are certainly an untapped resource with regard to screening for AF. As I mentioned, 90% of the population lives within 5 miles of a community pharmacy, and 90% of the population also visits a community pharmacy at least once a year. That's an opportunity at each of those visits to educate patients about the risks of AF and the risk and warning signs of stroke, for example, but also to screen for the asymptomatic AF. This is what we're really trying to approach—getting community pharmacists more involved.
Slide 22
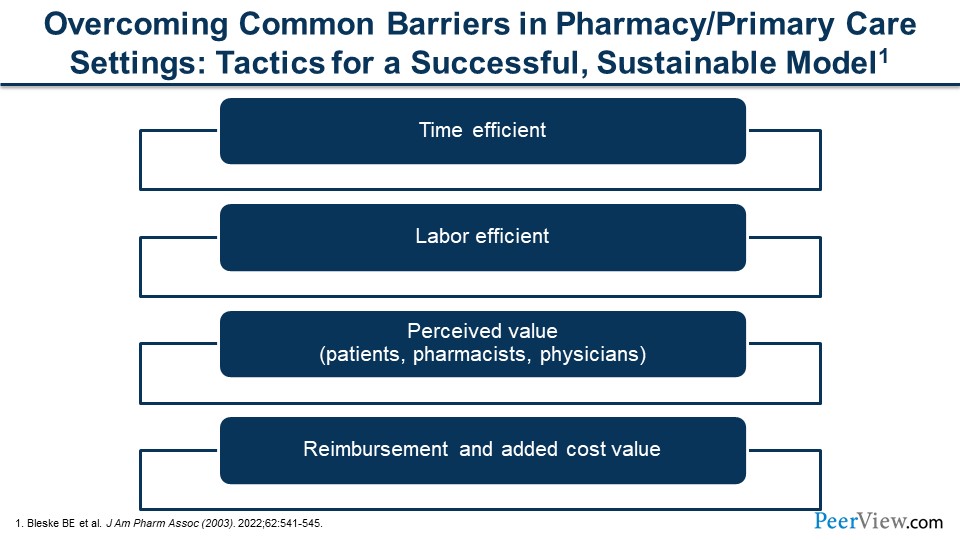
To do that, we have to have a sustainable model that can overcome some of the barriers that would be seen in the pharmacy setting or even the primary care setting. Any kind of screening that would be done needs to be time-efficient and labor-efficient. There has to be a perceived value for the patient to undergo these screenings or want to seek out these screenings, and there has to be a value for the pharmacist to provide these screenings. We want providers to see the value if a patient is screened in a pharmacy and comes into their office setting with a positive result and to understand what that means and that they should then pursue additional assessments of AF. In terms of cost, it has to be at least cost-neutral for pharmacies to be able to do the screenings.
Slide 23
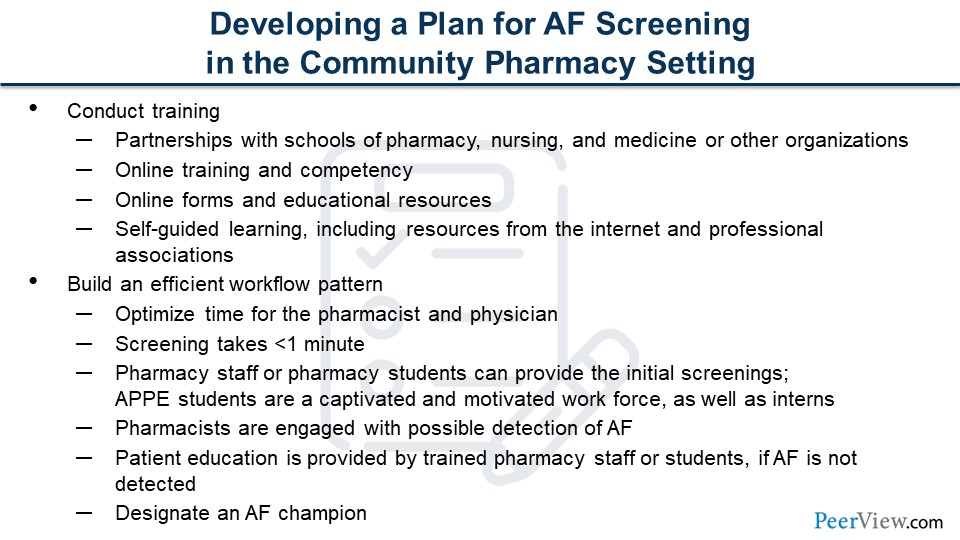
We would encourage community pharmacists to reach out to local colleges of pharmacy, maybe schools of nursing and schools of medicine as well. Many of them have online training programs that pharmacists can utilize for their staff. We have training at the University of New Mexico where we offer free CE training for pharmacy technicians and pharmacists. There are a lot of resources on the internet. The American Heart Association (AHA), for example, has numerous resources that individuals can go through and train on AF. What's really important for community pharmacists is to develop an efficient workflow pattern. We realize that pharmacies, pharmacists, and pharmacy staff are very busy. We understand that, but the screening really only takes less than 1 minute. If it becomes part of the routine workflow, it really does not add much additional time to normal work. We would encourage pharmacy staff to be trained on how to screen. It could be a clerk or it could be a technician. If the pharmacy has an intern, an intern certainly can do the screenings.
The pharmacists really just need to be engaged if there's possible AF in which they can talk to the patient to explain what AF is and what the risks are associated with it, and then importantly, encourage the patient to go see their primary care provider for additional tests and, ultimately, management of AF. And so, first and foremost, you have to have all your staff on board and trained with regard to screening for AF. We would say you should really designate an AF champion in your store, a person who's the go-to person for AF and can coordinate either these systematic or opportunistic screenings.
Slide 24
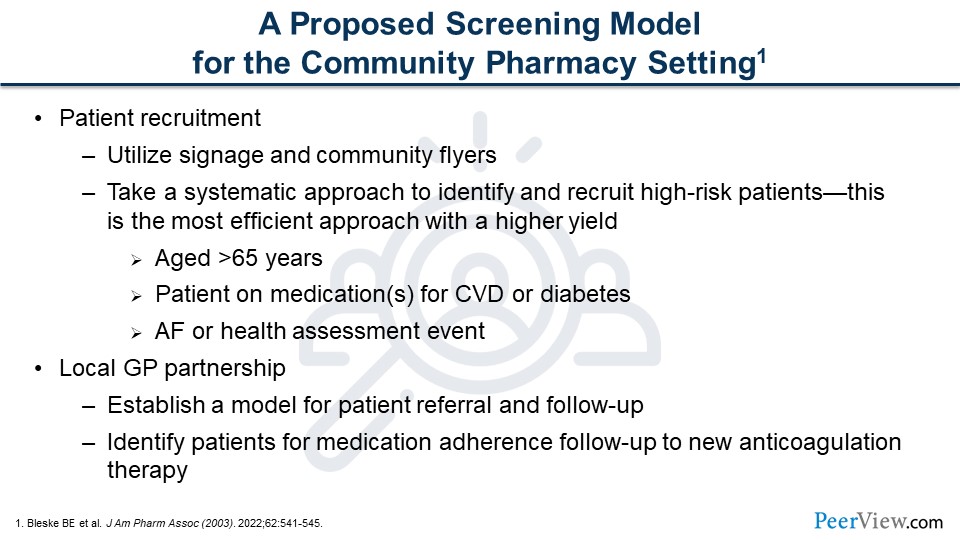
In terms of patient recruitment, we would simply say place signs around your pharmacy. We have signs we've created that read "Take 30 seconds to potentially save a life." That might capture a patient's attention and cause them to ask, you, "What is this? What is this about?" It's an opportunity to talk to them about the screening. If they're waiting for a prescription to be filled, screen them. Have your clerk or technician offer them some screening. It's important for community pharmacists to really partner with local primary care providers and talk to them about what it is you're doing, that you are periodically offering these screenings, and what it means when individuals get positive results. It's not a confirmation of AF, it's for the primary care provider then to follow up and do additional testing to determine if AF is present or not, and then what therapies to initiate.
Dr. Bleske: Joe, that's a really critical issue. You brought up a real critical point on establishing the collaboration with the local healthcare provider, especially in rural settings. Ash, can you talk a little bit more about this and how you see these collaborations perhaps coming together?
Dr. Achrekar: Yes; thanks for the question. This is a team approach. This kind of testing in the community—screening in the community—is very helpful as an initial step. But that's just the initial step. If AF is possibly found, collaboration with a general practitioner or primary care provider, or even a specialist, is essential. Those kinds of collaboration need to begin before the screening processes begin in the community pharmacy. I think Joe said it best: Collaboration with a school of pharmacy or a school of medicine is very helpful. That can be done telephonically via a teleconsultation and even through telemedicine. But collaboration needs to begin, so a patient, when screened in the pharmacy, has somewhere to go.
Slide 25
Dr. Anderson: Thanks, Ash and Barry. The other point I would talk about is the cost-effectiveness with this model. There is no model for reimbursement for doing these types of screenings; it's really a value-added service that a pharmacy is providing to their patients. Because of that service, hopefully it leads to retention of those patients as customers or clients of theirs. Periodically offering these screenings maybe three to four times a year or as we mentioned targeting more systematically higher-risk patients and offering those individuals screenings is cost-effective, because if you can prevent one stroke, that more than pays for itself.
Another value that pharmacies can accrue with this service is medication adherence—educating the patients about the importance of anticoagulation therapy and making sure that they're adhering to their therapy. Patients who take their medications—the drugs become more effective obviously—are also more reliable clients. They come back to the pharmacy, as we mentioned, multiple times. Additionally, the devices are very reasonable, under $200 to purchase one of these devices and set up a screening service.
Slide 26
At the University of New Mexico College of Pharmacy, we've taken many of these approaches and developed a sustainable and portable model for population screening for AF in the community setting. Barry, can you briefly describe this working model?
Dr. Bleske: Absolutely. So, as Joe mentioned, one of the models we use is working in student-driven health fairs, and we'll talk a little bit about how to perhaps set that up. The other approach we have taken, which is the health fair, is a more opportunistic approach. We've taken a very much more systematic approach in the community pharmacy setting. In this setting, we've established our APPE students and our P4 pharmacy students and have them screen patients. We do it in a systematic way, where we identify high-risk patients based on age and medication profile, looking for CV-type medications or diabetes-type medications. We have the APPE students perform the assessment. Our next level is going to be teaching pharmacy techs to do this. If no AF is reported, participants are counseled by the students on the results and we provide the education, and they're on their way. This is a time-efficient model. In this model, the pharmacist is not even involved in this process, so this is very efficient for the pharmacists.
If AF is reported, then the patients are counseled by both the pharmacist and the student. We ask permission to call their primary care physician to discuss the results with them and ideally set up an appointment. If patients don't want to do that, we give them a "Dear Doctor" postcard (an example of the postcard will be shown later and is available for download at www.PeerView.com/KMF). So, we explain the results and we counsel the patient on AF and stroke in general. We do this with an AHA flyer. Importantly, anyone who we screen gets this AF/stroke education, because we think it's important to provide the community with an avenue for stroke education and promoting stroke education, so individuals understand the risk for stroke and the signs and symptoms of stroke.
Slide 27
Dr. Bleske: Now, our model. We train our students and the pharmacists in the community settings to whom we're reaching out. We have online module training videos, competency exams, and hands-on training. As Joe mentioned earlier, we provide CE credit not only for pharmacists but for pharmacy technicians who are interested. As shown in the slide, there are instructions on how to log on. You're more than welcome to take the course and get CE credit for it. There's no charge for this. For our APPE students, it's a requirement. It's part of their APPE rotation. They have to do these assessments. Similar to medication adherence calls and patient counseling, it's part of the APPE experience. Data are reported back to the faculty champion and to our experiential office. The college provides the equipment, screening forms, signage and documents.
Slide 28
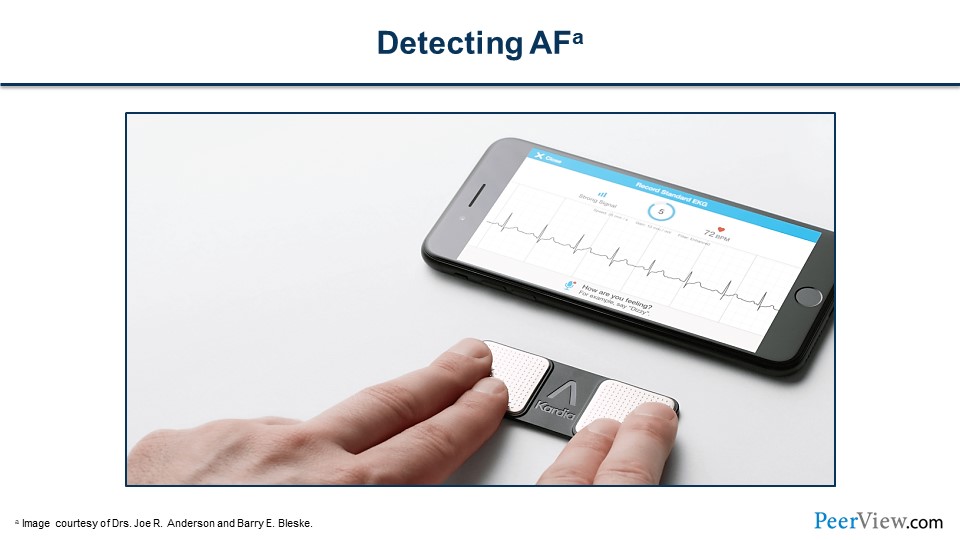
We use the Kardia mobile device, as shown in the slide. Again, in 30 seconds, we have a rhythm strip and an answer with it. It’s very efficient and easy to use. Patients also think it's kind of interesting.
Slide 29
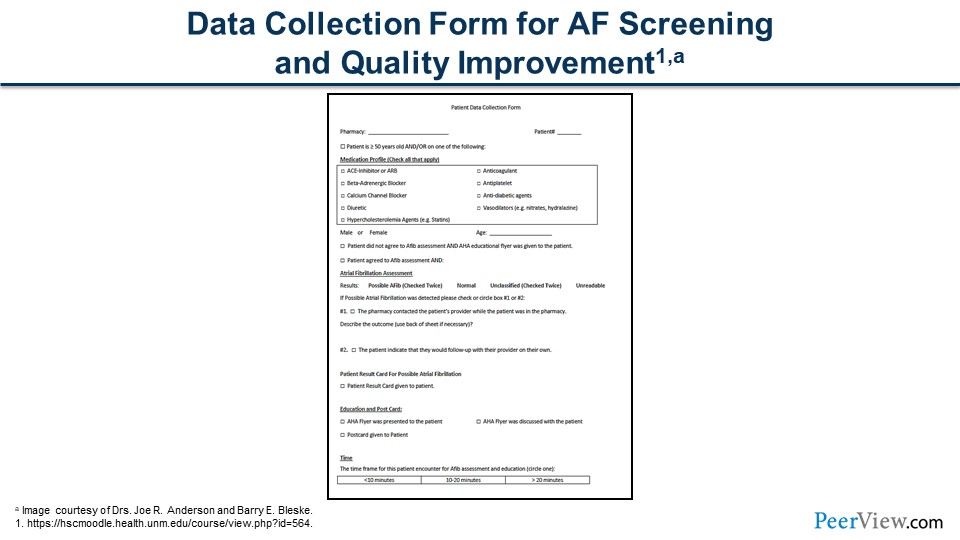
The slide shows our data collection form. It records our screening device, results, and time frame. And of note, when we see possible AF, we repeat the testing to make sure that we see it again.
Slide 30
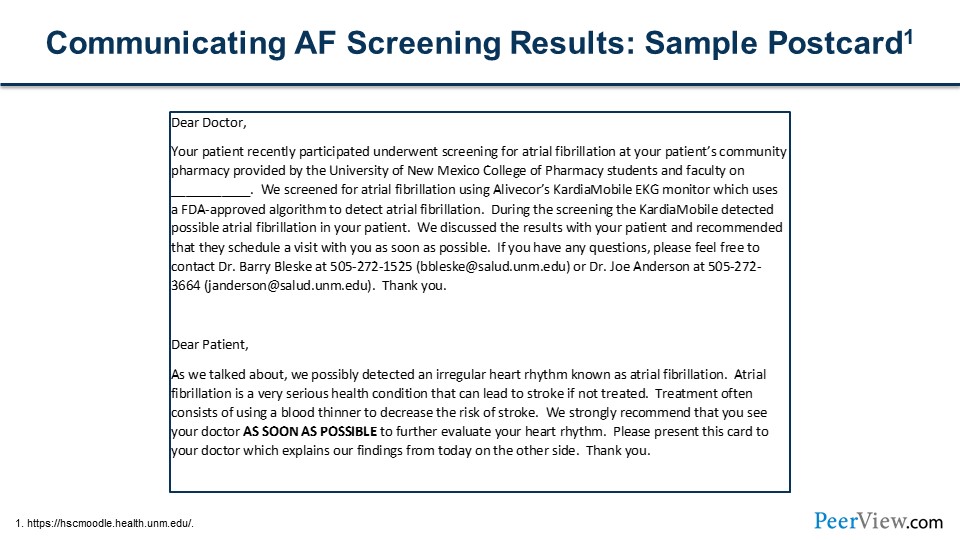
This slide shows our "Dear Doctor" postcard. It's a two-sided postcard. On one side, we tell the physician what we did, what device we used, the results we found, and our contact information, as well as how they could can contact us if they have questions. On the other side, we list the results in layman terms for the patient. Importantly, one of the things we counsel our patients on is getting a hold of their doctor as soon as possible to discuss the results that we found.
Slide 31
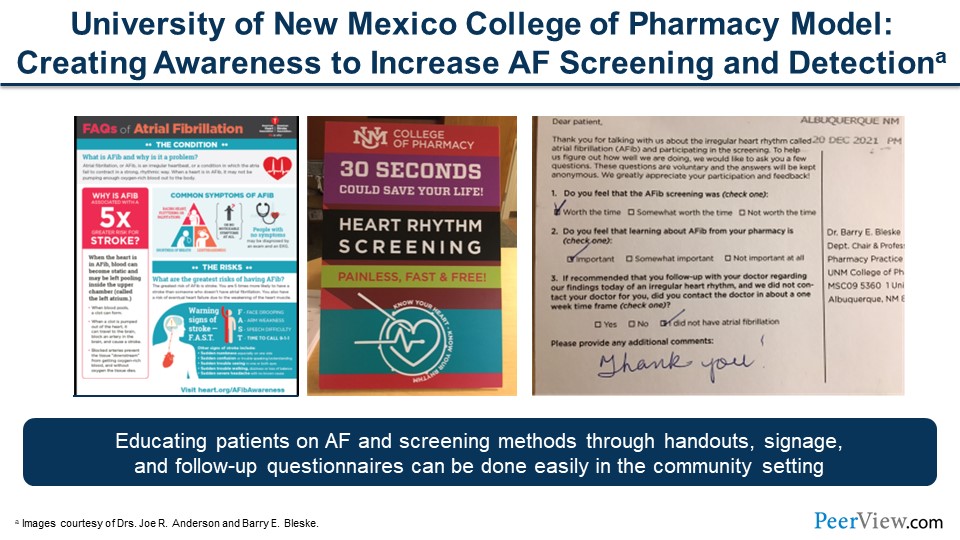
Some of the materials we use are presented on this slide. On the left-hand side is our patient handout; this comes from AHA. We download it. It is available in Spanish also. We go through this handout with every patient we see, and we talk about stroke and AF. We think this alone is a valuable service. The middle one image is what Joe had mentioned earlier and conveys the value of what we're doing. We give patients prepaid postcards to fill out and send back to us to get their assessment of what they think about this type of screening. As Joe also mentioned, we have signage we pass out to promote our "Know Your Heart, Know Your Rhythm" program.
Slide 32
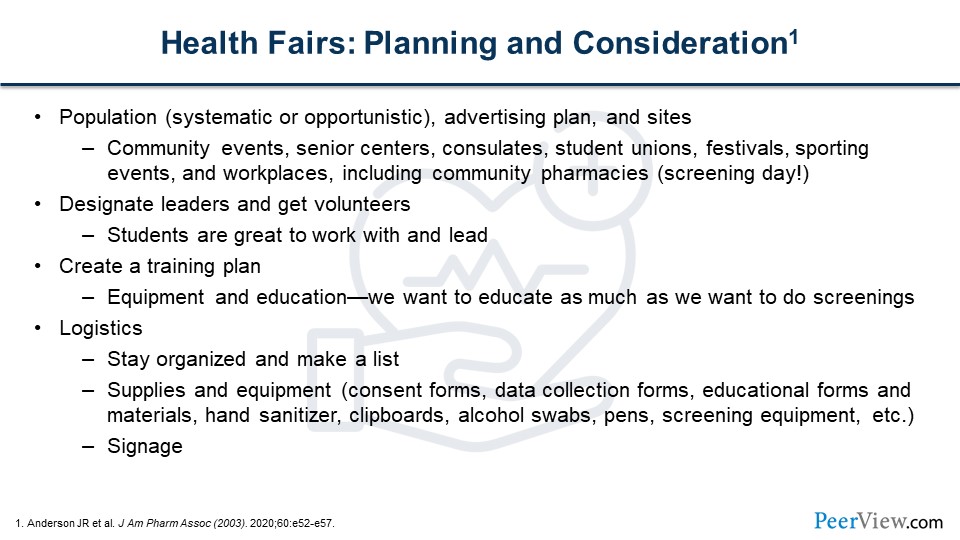
As I mentioned, another great opportunity that we've took advantage of is our student-driven health fairs. Going into the community, I say, is a great way to really connect with people. But there's a number of planning and other considerations needed when developing these events. One is: What kind of population do you want to target? Do you want a systematic or opportunistic approach? You've got to think about advertising, for example in the local paper, signage, and flyers. There are a lot of great places to do this, such as community events and senior centers. We've done it at consulates, student unions, and festivals. We were recently at the Lobos’ women's basketball game doing this, which was very successful. Workplaces are great, including community pharmacies. You can promote a screening day. By doing so, not only are you providing a service to the community but you're increasing your foot traffic into the pharmacies, which is also a good thing. It's important to designate a leader and make sure you get enough volunteers. Again, students are great to work with and they actually can lead this.
You want to make sure you have a good training plan. Remember to promote education; we're educating the public on AF and stroke. There are a lot of logistics involved as well. You've got to have supplies, equipment, chairs, tables, sanitizers, swabs, pens, signage, forms, and education materials. As part of this activity, we've provided a checklist for free download that we've developed and added onto to think about how to promote these community events. You can download these materials at www.PeerView.com/KMF.
Slide 33

Here are some pictures from our events. In the lower right-hand side, this is a photo from the Lobos women basketball game at the Pit. As you see, it was highly successful. We had BP screening, screening for diabetes, and AF screenings. The fans just loved it. On the left-hand side, we partner with Nagasaki University in Japan, and they are now doing this in Nagasaki Prefecture in Japan. That was at a shopping mall a couple years ago now, and we're going to go back in October to repeat this. Very exciting!
Slide 34
Joe mentioned this earlier. For these programs to be successful, people have to feel that there's a value to it. When we look at patient value, there are two studies in community pharmacies and one healthcare screening study that showed nearly 100% of patients were very satisfied or somewhat satisfied with the screening and they thought, importantly, that screenings were worth their time and were important. When we look at pharmacists' perception, they also felt it's a high value to the pharmacy. If you read some of those comments, it's a way to connect to customers in another way and to help patients in another way to contribute and to serve the community.
Slide 35
We talked about screenings in pharmacies and health fairs. I know we've alluded to this earlier but what about screenings in a clinical setting? Ash, is this feasible? Can we do this? What are your thoughts?
Dr. Achrekar: Thanks for the question. I think it's important. We've demonstrated that through the slides. However, 12-lead ECGs are often not done routinely in the clinic. There are reimbursement challenges. If somebody's complaining of symptoms, you can always do a 12-lead ECG. A new-onset of or asymptomatic AF obviously can be missed. As we discussed, only 50% of people feel when they're in AF. But this could possibly be circumvented if we screened patients in the waiting room. This would be a screening service gratis to patient with mobile devices while they're waiting to be seen.
I think it's probably important to establish a workflow pattern for every patient. Technology can be used, and this can be done with an MA or a nursing or pharmacy student at the point of care or during the initial assessment for each patient. Patients can even self-screen. There are downloadable apps and some patients will have mobile devices that they're wearing, such as smartphones. Obviously, there's still pulse palpation that can be used, and that's probably done in a clinical examination anyways. So, if AF is detected, a 12-lead ECG is appropriate at that time and laboratory testing, such as thyroid testing and some chemistries, can be ordered by the clinician as well. Confirmation's very important. Whether patients are screened in the pharmacy or in the waiting room, the results will have to be confirmed. In the next bit, we're going to talk about anticoagulation and appropriate therapies, as well as referring patients to an anticoagulation clinic.
Slide 36
Dr. Bleske: So we've talked a lot about screening by pharmacies, by clinics, by students, and by health professionals. Joe, can patients just screen themselves?
Dr. Anderson: Yeah, absolutely, Barry, they can. We've talked about all the different devices that are now available, and they're available not just for healthcare providers but for the general public as well. We know that the general public has these smartwatches. There are BP devices that can sense irregular rhythms. There's, of course, the handheld ECG devices that now are being marketed to individuals. So, yes, they can screen themselves. They can even do their own self-pulse check, and they can be educated on how to do that. But what's important for us as healthcare professionals to know is that these devices are out there. It's really important for us to educate our patients and the population that these are just screening devices. It’s also important to provide education about what is AF and the risks associated with it, and advise patients to seek out confirmation of the diagnosis with a primary care provider or a specialist. That's a critical piece, I think, in terms of following up with these patients who may be screening for themselves.
Pharmacy Call-to-Action: Implementing Collaborative Care Strategies to Manage and Engage Patients With NVAF
Slide 37
Dr. Bleske: There appears to be a tremendous opportunity to screen and to engage patients with AF. When patients do present with AF, we have to treat them. What should we as healthcare practitioners think about in regard to treating AF, Ash?
Dr. Achrekar: Thanks for the question. We'll briefly talk about treatment here. We talked about why it's important to treat AF; there's a fivefold increase in the risk of stroke and SE in both men and women. So all AFs must be assessed; after they are screened at the community pharmacy or at a health fair, then the results are confirmed by diagnosis, which is made by a clinician. We talk about three parts of AF treatment: rate control, how fast or slow the heart rate is; rhythm control, whether it's AF or normal sinus rhythm; and then finally, stroke prevention, which is probably the most important, because not only does it cause mortality but incredible morbidity as well.
Slide 38
The way we look at that is through scoring systems for stroke risk. Everybody doesn't have the same stroke risk. I told you all that I had AF when I was in medical school. It was a one-time event. It never came back. My CHADS2 score, or CHA2DS2-VASc score, was 0, which meant that my risk for having a stroke or SE was the same as the normal population. I didn't get any anticoagulation at that time. But there are two scoring systems that we use: the CHADS2 system and the CHA2DS2-VASc. We'll look at that in a little bit more detail, but these systems use selected clinical characteristics to predict the risk of stroke. All the scores provide a rough estimate of the risk of thrombosis or stroke in a population at a similar risk as the patient being reviewed.
Slide 39
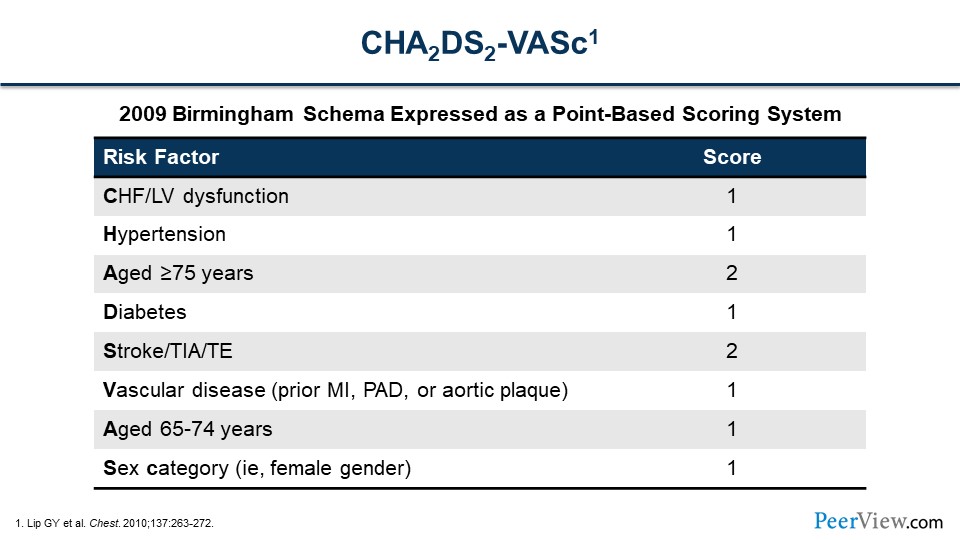
What that looks like is this. This combines both CHADS2 and CHA2DS2-VASc. As the slide shows, these risks increase your risk of stroke or SE. If you have congestive heart failure (CHF) with LV dysfunction, either an EF of less than 40% or a class II HF or worse, hypertension, aged 75 years or older, a history of diabetes and/or stroke—Stroke gives you a score of 2. We've extended that to a CHA2DS2-VASc scoring system that adds vascular disease, such as prior myocardial infarction, peripheral artery disease, or aortic plaque; a slightly lower age group there, with a lower score; and sex (female gender). The sex category's pretty important. Remember, we did look at the risk of women versus men developing stroke or SE. The female gender has a higher preponderance, if they have AF, developing stroke or SE, which is why there's an added point there.
Slide 40
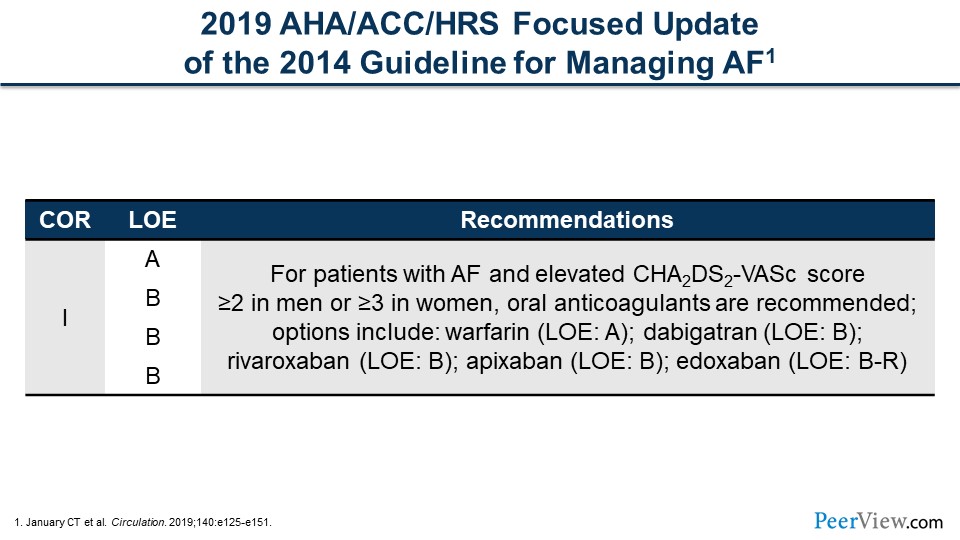
What that looks like from a guidelines perspective is in 2019 the AHA, the American College of Cardiology (ACC), and the Heart Rhythm Society (HRS) had an update to the AF management guidelines. So it's a class IA or B recommendation to treat AF with an anticoagulant in men with a CHA2DS2-VASc score of 2 or greater and women a score of 3 or greater. Warfarin, dabigatran, rivaroxaban, apixaban, and edoxaban are the recommended anticoagulants to prescribe.
Slide 41
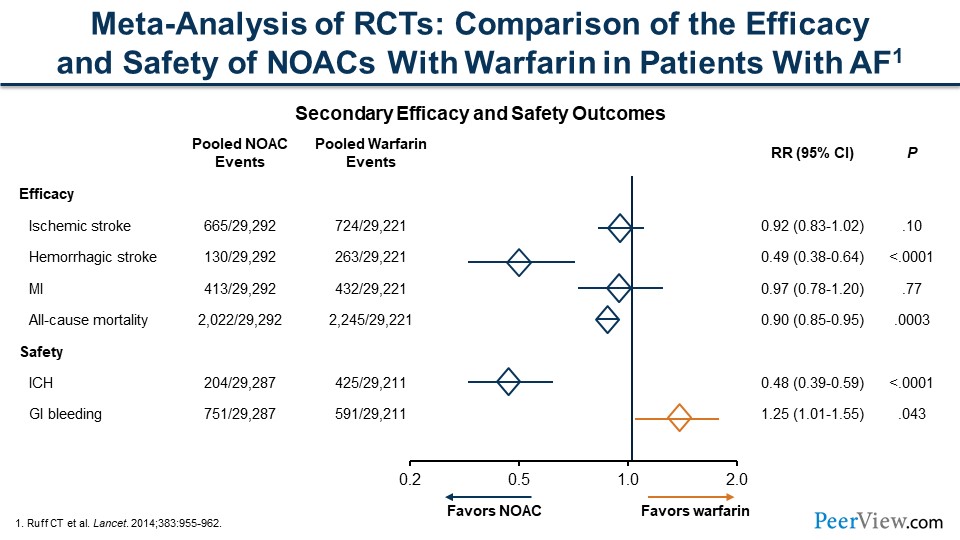
But all anticoagulants aren't equal, and over time we've had further data that shows that some anticoagulants are better than others. It's taken a while to collect these data. The true workhorse forever has been warfarin. This slide shows a comparison of the efficacy and safety of new oral anticoagulants, or novel oral anticoagulants (NOACs), with warfarin in patients with AF. These are meta-analyses of randomized trials, and a lot of the comparisons of the NOACs versus warfarin cross the line of unity. But we see a lot of safety in the NOACs. We can see a significant decrease in intracranial hemorrhage, as well as hemorrhagic stroke, when we're looking at the NOACs compared with warfarin.
Slide 42
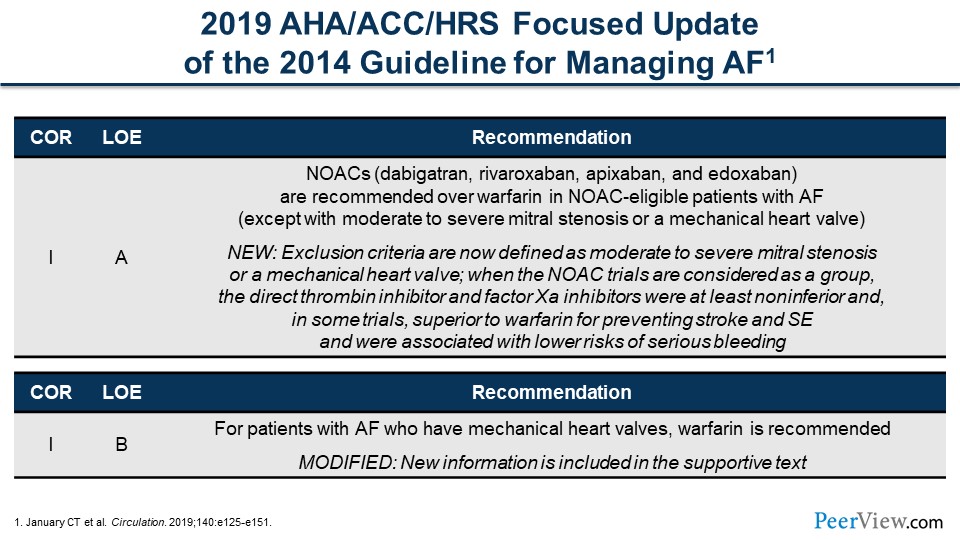
What that looks like from a guideline perspective is now it's a class IA recommendation to consider NOACs. Dabigatran, rivaroxaban, apixaban, and edoxaban are recommended over warfarin in patients who are eligible with AF. Remember, this is all nonvalvular AF (NVAF). In valvular AF, those patients who have moderate to severe mitral stenosis or a mechanical valve and those who still have an indication for treatment with anticoagulation, warfarin is recommended instead of one of the NOACs.
Slide 43
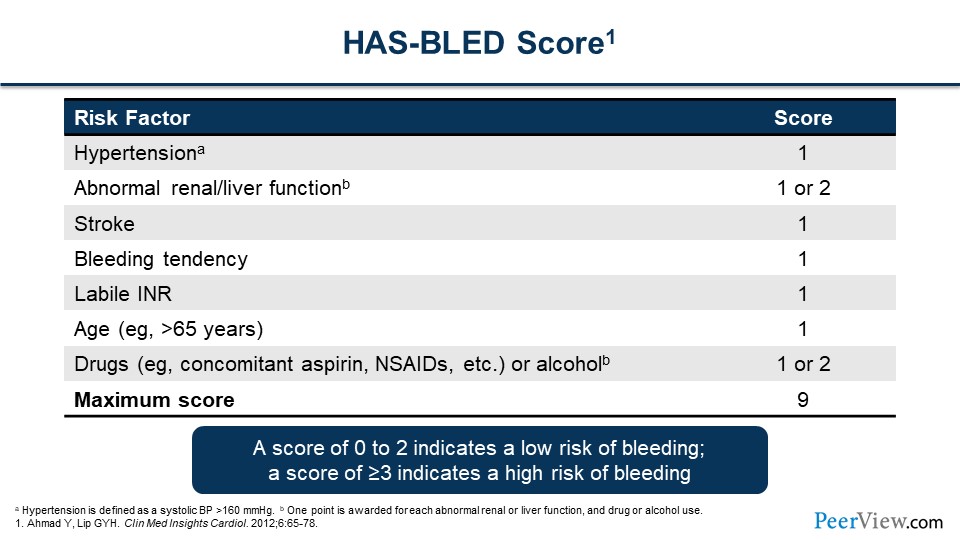
When we give patients an anticoagulant, we worry about two things. One, we want to thin their blood, as we say, to make sure that we reduce their chance of stroke or SE. But we don't want to overly thin their blood to the point of bleeding. We have a scoring system called HAS-BLED, and the table lists the risk factors. For those who practice medicine and the pharmacists out there, it doesn't seem very unusual that these risk factors would increase your chances of bleeding. Hypertension, abnormal kidney or liver function, previous stroke, bleeding tendencies, a previous history of labile INR, older age, concomitant drugs that actually have issues with bleeding as well, like NSAIDs and alcohol can be tabulated to a score.
Those with a greater score bleed more, while those with a score of 0 to 2 indicate a pretty low risk of bleeding. But a score greater than 3 indicates a risk of bleeding that's increased, and that increases as that score increases as well. What we really need to do is weigh the need for anticoagulation, likely with a NOAC for those with nonvalvular AF (NVAF) and balance that with the HAS-BLED score. The important part is that we treat these patients who are at higher risk.
Slide 44
Dr. Bleske: As you've pointed out nicely, there's a lot to consider when we're managing patients with AF, including risk factors and pharmacotherapeutic considerations. Ash, how do we approach patient-centered care from an interdisciplinary team perspective?
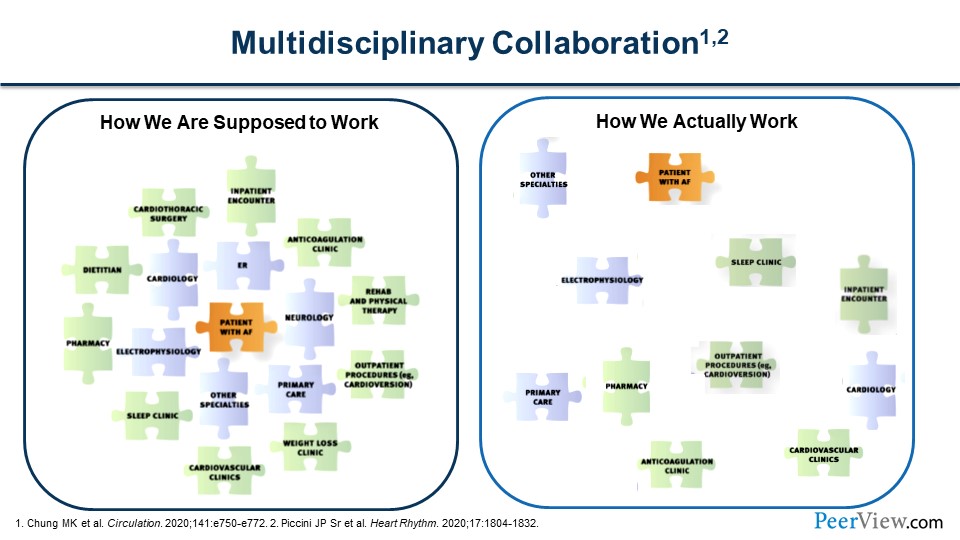
Dr. Achrekar: Thanks for the question, Barry. I think what we've demonstrated is that AF is going to be found in multiple settings. It can be found at a health fair, it can be found in an intensive care unit, and it can be found in cardiac rehab. The way we're actually working now is there's a lot of disparate care. On the right in this figure, you can see that the patient with AF is kind of floating around to these different clinics, whether it's electrophysiology, primary care, or community pharmacy. Many times, patients are actually diagnosed in a sleep clinic or at their sleep study, because they had an ongoing ECG throughout the night.
We need to replace this with a more coordinated care model. While the diagnosis, or at least the screening of AF, may occur in many settings and it will begin with the patient, we should have a more coordinated level of care among the patient and the various clinical settings. Those clinical settings are going to have to also be linked up with treatment settings, as well as our community pharmacies, to dispense those medications and follow those patients as well. If the screening happened at a community pharmacy, Joe and Barry are our pharmacists. I would think that that patient would be tied to that community pharmacy, and that the pharmacy has some commitment to that patient. I'm sure that the entire AF community would benefit from that as well.
Slide 45
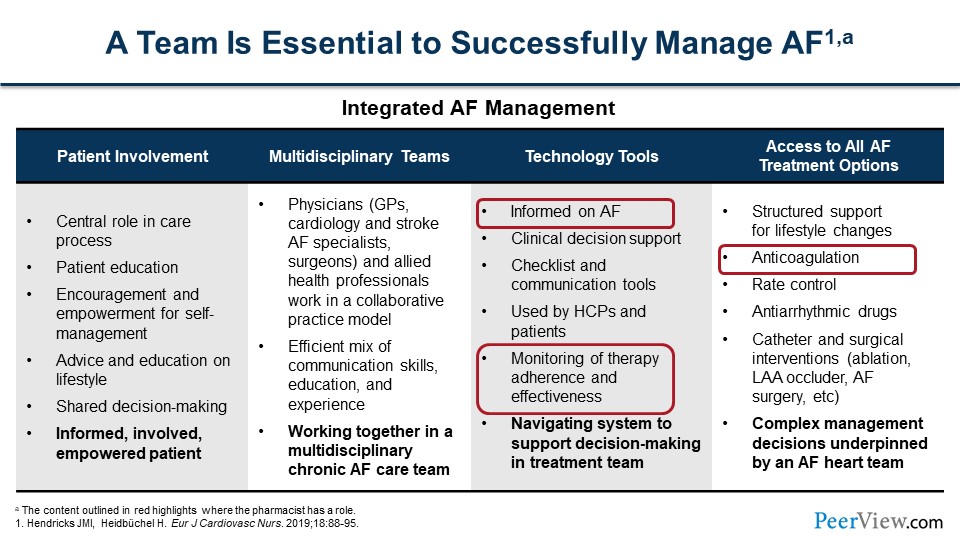
Dr. Bleske: Joe, this integrative, multidisciplinary team approach is really important. It involves many different type of services and professionals. Where do you see us, the pharmacists, having the greatest effect in this team setting?
Dr. Anderson: Thanks, Barry. As both you and Ash have alluded to previously, one of the roles of community pharmacists is just screening for AF using those devices and providing the opportunistic or systematic screening. But also, a really important role is just education. You touched on this earlier, Barry, but educating the patient about AF and what it is. If patients are performing the screening at home and they've got their own smartwatch informing them about the risks of AF and the importance of going and seeing their primary care provider for confirmation of the AF. Educating them about the risk of stroke is important. What are the warning signs of stroke and what should they do should they develop any of those warning signs? And then educating them about the treatments about which Ash spoke, whether it be rhythm control, rate control, or anticoagulation. What are those therapies, and why is it important to take those therapies? That goes along with another key role that is monitoring for adherence to therapy and making sure the patient is very adherent to that therapy.
Dr. Achrekar: I agree, Joe. It all begins with the patient. If the patients are educated, they'll have an idea of what that means, what the next steps are, and when they're screened, and if they screen in, following up with their clinician to determine what therapies are necessary. There are times that anticoagulation is not necessary. It's not very common, because AF is usually diagnosed in our older patients and anticoagulation is needed. But also, talking to the cardiologist or your primary care physician is important. There are some complex management issues that sometimes are necessary. But the first part is educating your patients, getting them diagnosed and following up with their clinician.
Dr. Bleske: As Ash and Joe have nicely discussed, we have to have an interdisciplinary team approach, because AF is complex.
Slide 46
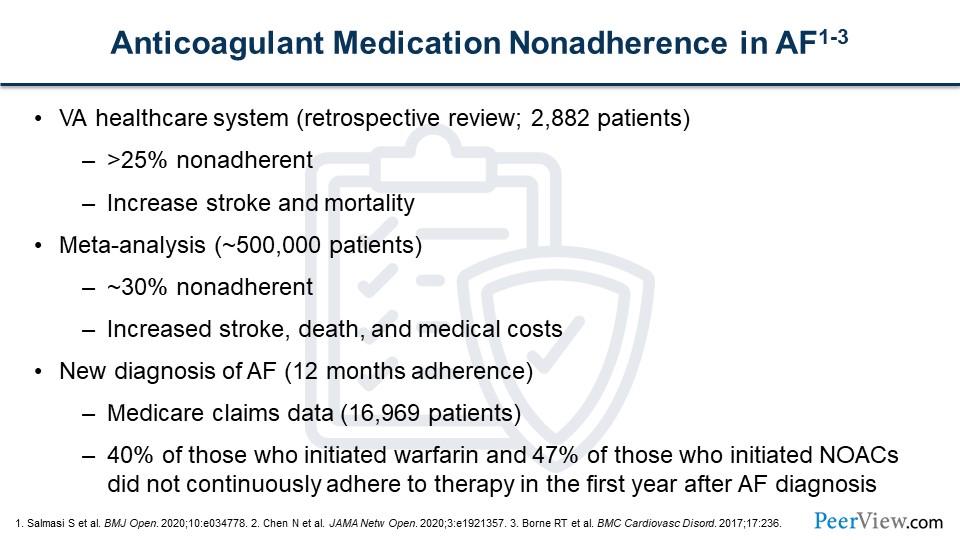
Now, another critical aspect that you've mentioned, Joe, is medication adherence. If patients don't take their medication, they're not going to prevent stroke associated with AF. Can you talk a little bit more about medication adherence, the importance of that in AF, and how do we improve, or what are the general factors on approaches to, medication adherence?
Dr. Anderson: Absolutely. Thank you, Barry. As you mentioned, if you're not taking your medication, it doesn't work. It's really important in regard to anticoagulation therapy, for example, because the greatest risk with AF is stroke. With proper anticoagulation therapy, we can reduce the risk of stroke anywhere from 40% to 80%, but you have to take the medication.
Studies, unfortunately, have shown that adherence rates with anticoagulation therapy vary, or I should say nonadherence rates vary anywhere from 25% to 40%. Importantly, in those studies, they're showing that in those patients who are nonadherent to their anticoagulant therapy, it does increase the risk of stroke and, unfortunately, the risk of death. Adherence to therapy is so very important.
Slide 47
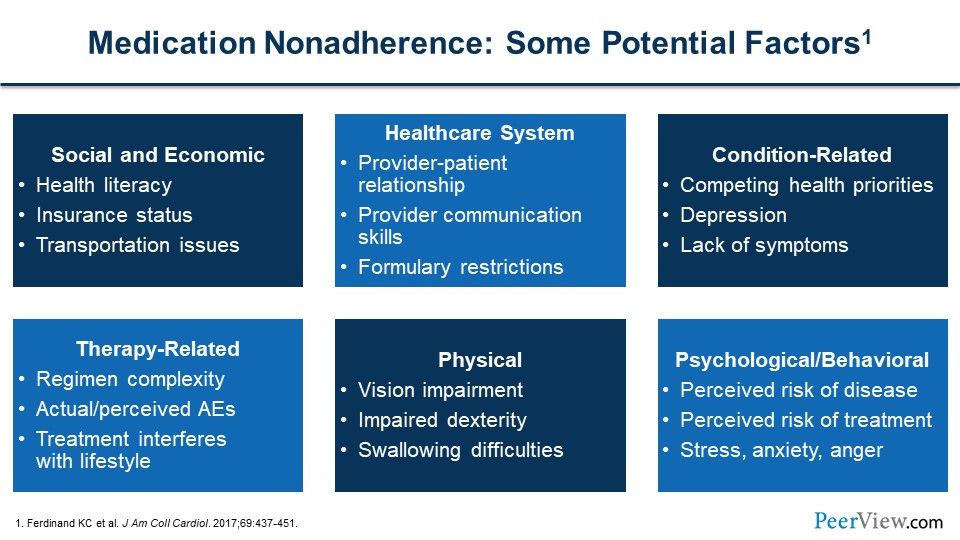
When we talk about medication adherence, or really any medical adherence, it's really a complex condition, if you will. There is a multitude of factors—many times multiple factors within one given patient. This slide goes over several of those potential factors for nonadherence, such as social and economic factors. Sometimes, patients have low health literacy levels, and so they may not be able to understand why they're taking a particular medication or how to take a particular medication. Insurance, sometimes, is a hurdle. If they don't have proper insurance, they may not be able to afford the newer anticoagulation medications or may not be able to afford transportation to get to their clinic appointments.
There are healthcare system factors. Studies show that if patients perceive a trusting relationship between themselves and their healthcare providers, they're more apt to adhere to therapy. They're more apt to come to their appointments. And so, proper communication plays a key role in improving adherence. There are also condition-related factors. We just talked about how AF is many times asymptomatic. Well, if you're asymptomatic and now you're asked to take a medication that has possible adverse effects and side effects, you may not be convinced of the need to take that medication. Once again, this goes back to the importance of communication and education with those patients. There, again, are a multitude of factors, sometimes physical factors, such as vision impairment, swallowing difficulties, trying to give them a formulation of the medication that they can take.
There may be some psychological factors involved as well, such as they don't perceive the risk of the condition or to exceed the risk of taking a medication. They may have seen on the internet that this medication can cause side effects. They may have seen commercials from lawyers asking them to call them if they've taken a particular medication. Naturally, they have an anxiety about taking that particular medication. Again, we have to overcome those concerns through education and communication with patients.
Slide 48
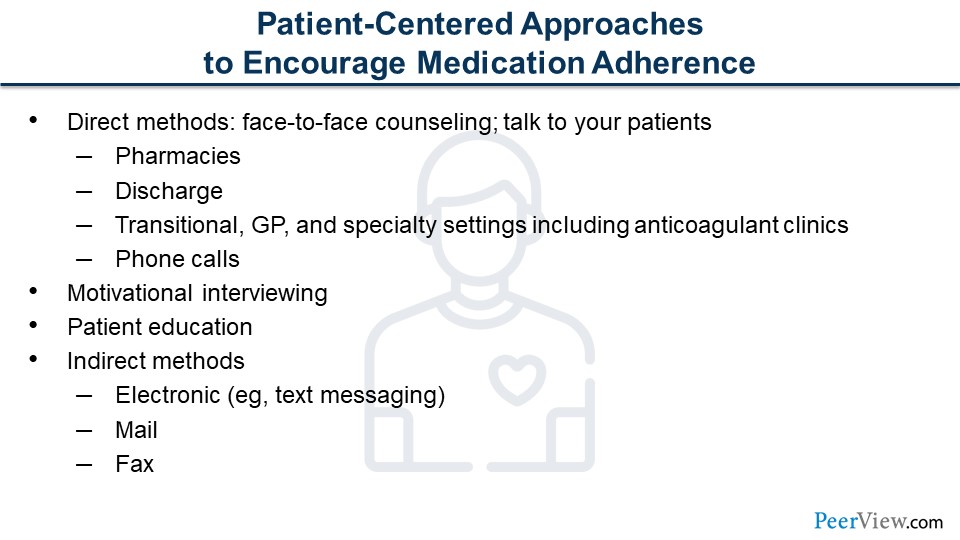
How do we overcome nonadherence? As I mentioned, talk to the patient. The key really is patient education. Ash mentioned it earlier; really talking to them about what the risks are with AF and how we can reduce those risks with proper treatment. There is a multitude of ways to communicate now. We talked about technology from a patient perspective, being able to screen oneself for AF. Well, now we have technology to communicate with patients. We can send text messages to them to say, "Hey, it’s time to come pick up your medication. We noticed you're late by a couple of days. Come on in and get your medication refill." There are those sorts of technologies.
Slide 49
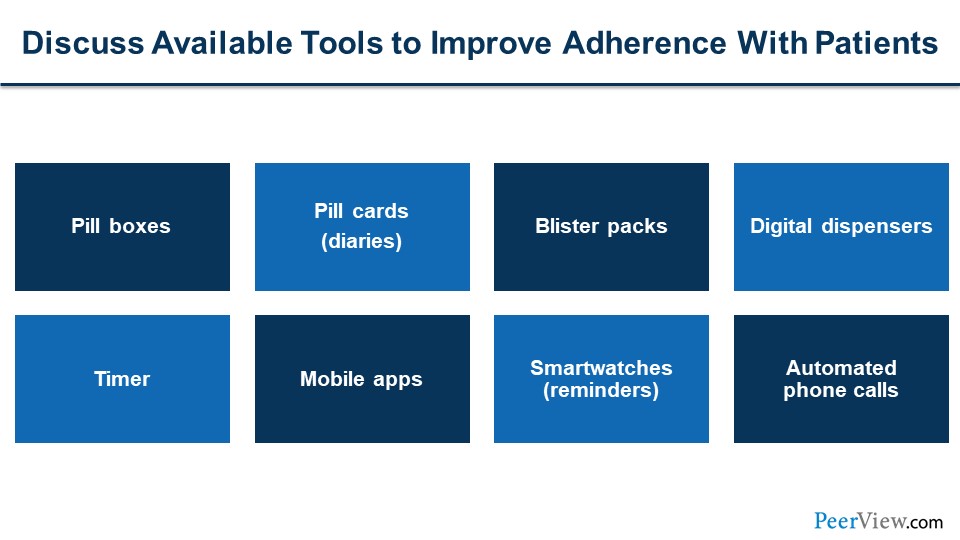
There are also simple pill boxes. They've been around for years but are vitally important. Ash mentioned earlier how he had AF, and fortunately, he did not have to take anticoagulation therapy. I've had illnesses, and unfortunately, I can't follow through on my therapy. I couldn’t remember to take it, so I have to have a pill box to remind myself to take medications. I think it's really important, and when you introduce other disease states and other medication therapies, it builds in terms of the ability to adhere to therapy. And so, it’s very important to implement pill boxes. Blister packs are great things. You can get as advanced as digital dispensers.
There are mobile apps now. You can educate your patients about what is a good app to utilize to remind them to take their medications. The smartwatches have built-in reminders and apps that they can use as well. Many pharmacies are using automated phone calls for adherence and refill reminders.
Slide 50
Continuing on with other approaches to improve adherence, we talked about the different settings of pharmacists. Pharmacists in the hospital settings are key for medication reconciliation. If a patient is diagnosed with AF in the hospital, now they have new medications that are being added as they're being discharged. What medications are they to continue upon discharge to their home, and what medications are they to discontinue? That's medication reconciliation, and that's an important role for all providers to make sure that patients are taking the appropriate medications they're supposed to take.
Simplifying medication regimens can help a great deal, such as once-daily dosing of medications. Many formulations now are available that are once daily. Obviously, adherence improves with once-daily medications versus twice or three times daily dosing. But really, telling the patient what medications they can take at the same time if they are taking medications multiple times a day. Ninety-day supplies can decrease transportation issues, for example, of coming in to the pharmacy once a month, as well as automatic refills where you time all their medications to refill at the same time, so they do not have to come back multiple times a month to get medications.
There's adherence packaging, as I mentioned. Those are things like the blister packaging where all their medications are packaged in a blister pack, so that they would take all their morning medications at once and all their evening or afternoon medications at once. These can all be helpful. Look for ways to reduce cost. Sometimes if cost is an issue for a particular patient, are there coupons that are available? Are there manufacturer programs in which the patient can be placed into to decrease cost? And of course, talking to patients about adverse effects, what to look for, and to notify you and/or their primary care provider should they have any of those adverse effects.
Slide 51
Dr. Bleske: Joe and Ash, that was a great overview. We talked about screening, diagnosis, and treatment, as well as the rationale for screening and why we should do it. We also discussed the concerns with asymptomatic AF and, importantly, not only treatment but also improving medication adherence in patients taking anticoagulants for AF. Now, as you both clearly pointed out, we have to work collaboratively with our clinical colleagues to really move patients through the system and bridge the gap between patients and all members of the healthcare team to improve AF screening, diagnosis and importantly treatment. Again, we can't emphasize this enough, especially being pharmacists, medication adherence is critical.
Before concluding the program, make sure you review and download the resources that we've provided at www.PeerView.com/KMF. Please feel free to share them. We think this is important, and we're more than happy to have this information disseminated out to other healthcare practitioners to help with screening and managing AF. And with that, our discussion for today ends. Thank you, again, Joe and Ash. You both shared great insights today, and we all hope you found this activity informative and useful to your practice.
Back Top