ADVERTISEMENT

Compounding Preparations for Ophthalmic Use in Humans
INTRODUCTION
The human eye—an organ that is exposed to the ambient environment—theoretically should allow easy access to administer medications. Actually, the eye's structure resists administration of topical ophthalmic medications. Compounders, pharmacists, and pharmacy technicians need to be familiar with eye anatomy and ophthalmic preparations' components to choose and/or develop the best dosage form to treat various ocular disease states.
Eye Anatomy
The eye is essentially divided into 2 segments: anterior and posterior.1 The eye's anterior segment provides the organ's first line of defense for preventing injury. Its primary barrier is the clear cornea and its 3 layers: epithelium, stroma, and endothelium. The epithelium and endothelium layers are lipophilic and resist absorption of aqueous or water-based substances.1 The epithelium, the cornea's outer layer, comprises 90% of corneal cells. It is a tightly bound structure, which makes it very resistant to aqueous and hydrophilic substances. Although the endothelium, the inner layer, is also lipophilic, it is a single layer of porous cells that allows molecules to pass into the eye's anterior chamber.1
The stroma—the middle and thickest layer of the cornea—is hydrophilic. It is a highly organized network of collagen fibrils, which creates the eye's mechanical strength and transparency.1 The Bowmen's membrane is also part of this hydrophilic layer and is located between the epithelium and the stroma.2 The sclera or "white of the eye" is also hydrophilic and has permeability similar to the corneal stroma.
The posterior segment comprises the eye's back two-thirds and includes the vitreous humor, retina, choroid, and optic nerve. These components are primarily responsible for vision.1
The eye's lacrimal system, another major component, produces tears. The lacrimal system consists of lacrimal glands, lacrimal canals, a lacrimal sac, and a nasal lacrimal duct.1 Tears contain mucin, which forms a hydrophilic layer over the corneal surface. This layer lubricates the eye and flushes debris and pathogens. Tears have a pH of 7.4 and are isotonic. The tear volume in humans is 7 mcL to 9 mcL; however, the cul-de-sac or drainage canal of the upper and lower eyelids contains 20 mcL to 30 mcL of tears. The tear film's restoration time is 2 to 3 minutes. Blood capillaries and lymphatics are located in the conjunctiva. Drugs can be systemically absorbed in the conjunctiva, which significantly lowers the drugs' availability locally to the eye.1
OPHTHALMIC MEDICATION DRUG DELIVERY SYSTEMS
An ophthalmic drug delivery system's goal is to achieve a therapeutic concentration of the active drug in the target tissue for an appropriate duration. For example, an inflammatory condition in the eye's posterior segment probably cannot be treated effectively with a topical anti-inflammatory ophthalmic solution. It may require a more invasive treatment such as an intra-ocular injection. However, patients or caregivers can treat superficial corneal abrasions effectively with topical ophthalmic solutions or ointments. Selection of an ophthalmic dosage form is dependent on the eye's affected part, the drug's chemical and physical properties, and patient compliance. Ideally, a medication drug delivery system for ophthalmic preparations should include the following characteristics3:
- It should not induce a foreign-body sensation or long-lasting burning.
- It should not cause blurred vision for extended periods of time.
- It should act locally rather than systemically.
- It should be easy to administer.
- Administration frequency should be kept to a minimum to improve patient compliance.
Topical Dosage Forms
Topical ophthalmic dosage forms (solutions, suspensions, and ointments) are the most commonly prepared and used dosage forms for the eye. Patients or caregivers can administer them easily and they treat most diseases or conditions of the external eye or anterior segment effectively. Since very little drug reaches the vitreous humor, these dosage forms are poor options for treating diseases affecting the eye's posterior segment (e.g., macular degeneration). The drug's effectiveness and ability to reach its target tissue site depends upon3:
- The condition of the cornea and anatomical barriers of the eye
- The pharmacodynamics of the tear film
- The physical properties of the drug and its vehicle
- The drug's bioavailability
There are 2 types of topical ophthalmic liquids: aqueous and nonaqueous. Aqueous solutions are quickly absorbed and affect the patient's vision minimally. Aqueous solutions also do not interfere with practitioners' instruments during examinations or procedures. They have brief therapeutic effect and are good dosage forms for diagnostic procedures; however, they are poor treatment choices for chronic conditions. Medications in aqueous vehicles, such as antibiotics, require frequent administration to be effective. Most topical solutions are washed away by tears within 15 to 30 seconds of administration; less than 5% of the dose actually reaches the eye's posterior segment.4 Aqueous ophthalmic suspensions may be used to prolong drug effects. The active drug, located in the particles, slowly dissolves and releases over time. Topical aqueous ophthalmic liquids' disadvantage is their systemic absorption by the alimentary tract after the liquid drains through the nasolacrimal duct.3
An advantage of nonaqueous or "oily" ophthalmic solutions is that they form a film over the eye, allowing longer drug contact.1 The film reduces drainage and decreases risk of systemic drug toxicity. The film also acts as an emollient and keeps the eye moist, which helps irritated and dry eyes. An oil-based solution, which lacks water, can increase the stability of a drug that is easily degraded by hydrolysis. Nonaqueous solutions' disadvantages include blurred vision and interference with practitioners' instruments.5
Topical ophthalmic ointments also contain no water; they are good vehicles for drugs that are unstable in aqueous solutions and undergo rapid hydrolysis.4 Adding an active drug to an ophthalmic ointment base offers multiple advantages. It prolongs contact of the drug with the eye; provides slow, continuous absorption; and requires less frequent administration than aqueous topical solutions. These dosage forms are safer for drugs that have narrow therapeutic windows (e.g., atropine). Ophthalmic ointments are often administered at bedtime to minimize interference with the patient's vision. Topical ophthalmic ointments offer the same advantages as nonaqueous solutions and treat chronic conditions well. The disadvantages are also the same, such as blurred vision.4
Ophthalmic ointments are also prepared without any active drugs. They are used in trauma patients as a nonirritating, protective agent. These bland ophthalmic ointments also have no adverse effect on corneal wound healing.6
Drugs commonly used in topical ophthalmic dosage forms include antibiotics, antifungals, anesthetics, steroids, dyes, and agents to treat chemical burns. Antibiotics and antifungals are used to treat acute superficial eye infections. Calcium gluconate and ascorbic acid are used to treat chemical burns to the cornea.7,8 Cocaine is compounded off-label as an ophthalmic solution for anesthesia. Hyaluronidase ophthalmic solution is used off-label as an adjuvant for retrobulbar/peribulbar block.9,10
Cyclosporine is compounded in corn oil as a 2% nonaqueous solution and used off-label to prevent corneal immune graft rejection when used with topical ophthalmic steroid solutions. It is also used to treat vernal keratoconjunctivitis (KCS) or chronic graft-versus-host disease with KCS .11,12 The commercial product, Restasis or cyclosporine ophthalmic emulsion 0.05%, has an oily emulsion base which serves 2 purposes: it is an emollient and it keeps the active drug in contact with the eye to help reduce inflammation due to chronic dry eye.13
Erythromycin ophthalmic ointment is administered to newborns at birth to prevent ophthalmia neonatorum (contracted during passage through the birth canal from a mother infected with either Neisseria gonorrhoeae or Chlamydia trachomatis).14 Rose bengal is compounded into a 1% solution as a diagnostic aid for practitioners to diagnose various ocular injuries.15
Ocular Injections
Although ocular injections are invasive, uncomfortable, and inconvenient for patients, they may be indicated to treat inflammatory conditions of the eye, severe infections, macular degeneration, and to provide prophylaxis and anesthesia for ophthalmic surgical procedures. Ocular injections can provide a therapeutic drug dose for an extended period of time and may be preferred for ophthalmic conditions involving the eye's posterior segment. Different types of ocular injections target different eye areas: conjunctival, intravitreal, peribulbar, retrobulbar, subconjunctival, intracameral, and sub-Tenon's.16 The common ocular and periocular injections are intravitreal and subconjunctival. Figure 1 illustrates the administration of sub-Tenon's and intravitreal injections.
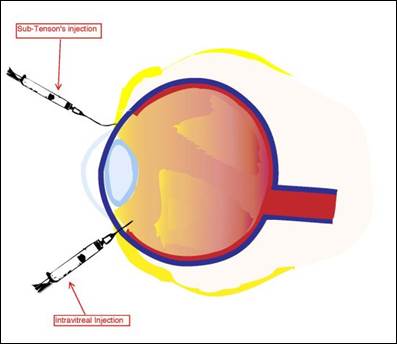
Figure 1. Administration of sub-Tenon's and Intravitreal Injections.
Diagram from the National Eye Institute, Reference 2.
Periocular injections, such as subconjunctival and sub-Tenon's or episcleral space, are used to bypass the eye's anterior segment's physical barriers. Subconjunctival injections are injected underneath the conjunctiva, while sub-Tenon's injections are administered in the cavity between the Tenon's capsule and the sclera.17,18 These injections are typically used to administer antibiotics, corticosteroids, and mydriatics after a surgical procedure or in acute inflammatory conditions of the anterior segment. Although not the first line of therapy, subconjunctival injections are used to administer steroids in treating recalcitrant anterior and posterior uveitis. Subconjunctival injections deliver steroids to the eye steadily because the lipid-soluble steroid moves from the conjunctiva to the tear film where it is absorbed through the cornea. Both the subconjunctival and sub-Tenon's injection have similar dosing volumes, about 0.5 mL. Although periocular injections can be very effective, potential complications from administration include subconjunctival hemorrhage, pain, irritation, induced intraocular pressure spikes with steroids, secondary infections, chemosis, ecchymosis, perforation of the eye globe, and retained drug deposits.19
Intraocular injections are administered directly into the eye's globe and posterior segment to ensure the drug reaches the target site. Intracameral injections are injected into the eye's aqueous humor, and intravitreal injections are injected into the eye's vitreous humor. Both injection types treat severe infections and emergent conditions, such as endophthalmitis. Due to the dosage forms' invasiveness, these injections are administered in a sterile clinical setting or operating room under local anesthesia. Dosing volume is usually 0.1 mL.17,18
The use of intravitreal injections has significantly increased since the 1970s and offer therapeutic advantages similar to periocular injections.16 Complications may include intraocular hemorrhage, pain, irritation, induced intraocular pressure spike, secondary infection, optic nerve damage, retinal detachment, and uveitis or iritis. Drugs commonly administered intravitreally include antibiotics and antivirals, antiinflammatories, antineoplastics, and endothelial growth factor inhibitors. These drugs are therapy's mainstay for ophthalmology and are used to treat endophthalmitis, viral retinitis, age-related macular degeneration, diabetic retinopathy, uveitis, vascular occlusions, and retinal detachment.20,21
COMPONENTS IN OPHTHALMIC PREPARATIONS
Components or ingredients other than the active pharmaceutical ingredient and vehicle used in ophthalmic preparations or products are necessary to make stable, effective, and comfortable ophthalmic dosage forms.22,23 Several factors must be considered when compounding ophthalmic preparations: chemical stability of the active drug(s), possible microbial contamination, incompatibilities, viscosity, pH and buffering, tonicity, particle size (if a suspension), final container (such as dropper bottle or syringe), compatibility with the eyes, appropriateness of the vehicle, and patient comfort and tolerability. Each component or ingredient should be assessed for compatibility with other components or ingredients in the ophthalmic preparation. The Handbook of Pharmaceutical Excipients contains detailed information about raw ingredients mentioned in the above sections, which should be consulted for a more detailed review.23
Preservatives
If possible, all multidose containers should contain a preservative to prevent microbial contamination during use.21 Preservatives often used in ophthalmic preparations and commercial products include benzalkonium chloride (BAK), chlorobutanol, benzethonium chloride, phenylmercuric nitrate, phenylmercuric acetate, and thimerosal. Table 1 lists these common preservatives and the usual effective concentrations.21 BAK and thimerosal are the most commonly used preservatives for ophthalmic preparations and products. BAK has a broad range of activity against a variety of bacteria, yeast, and fungi, but works the best against gram-positive bacteria. Solutions with BAK remain stable over a wide range of pHs and temperatures without losing anti-microbial effectiveness. Some patients do, however, develop an allergy to BAK and may need their ophthalmic medication prepared without it. Soft contact lens wearers should avoid solutions with BAK because it binds to the hydrogel.
| Table 1. Preservatives Used in Ophthalmic Preparations and Usual Concentrations |
| Preservative |
Usual Concentration (% w/v) |
| Benzalkonium Chloride |
0.013 |
| Benzethonium Chloride |
0.01 |
| Chlorobutanol |
0.25 to 0.5 |
| Phenylmercuric acetate |
0.004 |
| Phenylmercuric nitrate |
0.004 |
| Thimerosal |
0.01 |
| Abbreviation: w/v = weight to volume Source: Reference 21 |
Thimerosal is the alternative preservative to BAK and can be used by soft contact lens wearers. It is bacteriostatic and fungistatic at neutral and alkaline pHs, but bactericidal at acidic pH levels. Although it is stable at room temperature, it is also light sensitive.21
All preservatives have drug incompatibilities and a compounder must ensure the chosen preservative is compatible with all components in the ophthalmic dosage form. All ocular injections must be prepared without preservatives, which can be toxic to the eye's internal structures, especially when injected.24,25
Antioxidants
Antioxidants are added to ophthalmic preparations when the active drug is susceptible to oxidation or degradation by free radicals. In other words, antioxidants stabilize the drug. Common antioxidants include ethylenediaminetetraacetic acid (more commonly known as edetate disodium [EDTA]), sodium metabisulfite, and sodium bisulfite. EDTA can also be used as an adjunct with BAK to enhance BAK's antimicrobial activity. Sodium metabisulfite is useful in acidic solutions, whereas sodium bisulfite is used in neutral pH solutions.22
Viscosity Agents
Viscosity agents thicken ophthalmic liquid vehicles, especially aqueous solutions, to increase contact time of the drug with the eye and minimize drainage into the nasolarimal system. Viscosity increases drug absorption and therapeutic effects. The viscosity of ophthalmic solutions ranges from 25 centipoise (cps) to 50 cps. Viscosity agents must usually be sterilized by autoclaving before addition to an ophthalmic preparation because they cannot be sterilized through filtration. Commonly used viscosity agents include hydroxyethylcellulose, hydroxypropyl methylcellulose (HPMC) or hypromellose, methylcellulose, polyvinyl alcohol (PVA), and polyvinyl pyrrolidione or povidone. PVA is commonly used in artificial tears and contact lens solutions, and is stable at temperatures below 100°C. HPMC is preferred over methylcellulose because it produces solutions with greater clarity and has soothing and lubricating properties.26
Tonicity Agents
Since human tears are isotonic and very similar to 0.9% sodium chloride solution, it was thought that tonicity was important for ophthalmic preparations. However, the eye tolerates tonicity ranging from 0.6% to 1.8%. From a practical viewpoint, patients generally tolerate hypertonic solutions very well. Although the ideal osmolality value is 300 mOsm/L, most patients can tolerate an osmolality range of 200 mOsm/L to 600 mOsm/L. Only vehicles and lubricating solutions, such as artificial tears, must be isotonic. Common tonicity agents include dextrose, glycerin, and sodium chloride. Occasionally, a patient cannot tolerate a hypertonic solution because the active ingredient's sodium value is too high. If it is impossible to make the solution within an acceptable tonicity range, a viscosity agent may reduce some of the patient's pain and discomfort.26
Clarifying Agents
All ophthalmic solutions should be free and clear of any particulate matter to prevent abrasions to the cornea or eyelid. Filtering solutions through a 0.4 micron filter should remove all particulate matter without removing the drug. Using HPMC can serve a dual purpose in ophthalmic preparations. Not only is it a viscosity agent, but HPMC can improve the ophthalmic solution's clarity. Polysorbates, e.g., polysorbate 20 and polysorbate 80, can also improve clarity because these agents act as solubilizing agents to help dissolve poorly soluble ingredients.26
pH and Buffering Agents
The pH can affect the chemical stability, potency, and effectiveness of drugs and components in a dosage form. An optimum pH avoids adverse effects, ensures that drugs will produce an optimum therapeutic effect, and ensures all components' roles are optimized. For example, most drugs are acidic or neutral and will precipitate, rendering the drugs inactive if added to a basic solution or vehicle. A precipitate in an ophthalmic preparation could also potentially cause an corneal abrasion. Some preservatives' antimicrobial activity may be decreased if the pH is incompatible with the preservative. As mentioned previously, thimerosal is bacteriostatic in neutral or basic pHs, but bactericidal in acidic pHs.
Buffers are used in ophthalmics when the pH is critical and must be within a certain range. Buffering agents are designed to maintain a certain pH throughout the preparation's shelf life. The system's buffer capacity allows the tears' buffer system to bring the administered solution back to the tears' pH. Ideally the buffer capacity should be less than 0.05 and maintain a pH range of 4 to 8. Ophthalmic buffering agents are usually citrate, phosphate, or acetate buffers.26
Vehicles and Bases
Most vehicles and bases used in compounded ophthalmic preparations are commercially available, isotonic mixtures and may contain preservatives. Depending on the dosage form and indication, the vehicle or base may contain lubricants, wetting agents or demulcents, electrolytes, viscosity agents, or buffering systems. It is very important when preparing compounded ophthalmic medications to ensure that the vehicle or base is compatible with all of the formula's active pharmaceutical ingredients and components. There are basically 2 types of vehicles and bases: aqueous and oleaginous or nonaqueous.22
Aqueous vehicles and bases are primarily used for topical solutions and ocular injections. It is very common to use commercial balanced salt solutions or artificial tears as a vehicle for topical solutions; however, different brands differ in content and may not be interchangeable. Dextrose 5% in water for injection has been used as a vehicle for vancomycin 50 mg/mL ophthalmic solution and reported by patients as comfortable when administered.27 If a formula for an ophthalmic preparation is based on a published stability study, the compounder must replicate the study formula exactly (i.e., use exactly the same brands or generics the study used) if they plan to assign the beyond-use dating (BUD) established in the study. For example, if a stability study indicates it used the Systane brand of artificial tears, compounders cannot substitute another brand, like Murine Tears, and assign the BUD established in the study. Systane contains polyethylene glycol 400 and propylene glycol, whereas Murine Tears contains polyvinyl alcohol and povidone. These brands are not equivalent or interchangeable even though they are both artificial tear solutions. Prior to mixing and assigning a BUD, compounders must review the vehicles' contents to determine the compatibility of the active ingredients and components in a compounded ophthalmic formula.22
Ocular injections must be prepared with preservative-free diluents, such as 0.9% sodium chloride solution for injection, sterile water for injection, or 5% dextrose solution for injection. These solutions may also be used to prepare topical solutions.26
Oleaginous vehicles and bases are primarily used to prepare ophthalmic topical ointments or topical "oily" solutions. When commercial ointments are used, all of the ophthalmic formulation's components need to have been individually sterilized before mixing since an ointment cannot be filtered through a 0.22 micron filter. Nonsterile ointment bases can only be sterilized by dry heat. Autoclaves sterilize by a combination of heat and pressure to create steam. Since an ointment contains no water, no steam is generated to sterilize it. Bland lubricating ophthalmic ointments that do not have active ingredients consist of 3 basic ingredients in various concentrations: white petrolatum, mineral oil, and lanolin.28 All of these ingredients are nonirritating and safe for use in the eye. Yellow petrolatum is not used in ophthalmic preparations because it is less purified than the white petrolatum and can be more irritating to the patient. For topical "oily" solutions, some fixed oils, such as corn oil or medium chain triglycerides oil, are also safe to use and can be sterilized by filtration through a 0.22 micron filter or with dry-heat.28
Active Pharmaceutical Ingredients
Ophthalmic drugs are used to prevent or treat eye diseases, relieve uncomfortable symptoms that a patient may experience, or to aid practitioners in ophthalmic diagnostic procedures. Active pharmaceutical ingredients (APIs) may be obtained from commercial sterile products, such as parenterals, nonsterile bulk powders, or liquids. Most compounded ophthalmics can be prepared with commercial sterile products; however, some compounders may need to prepare them using non-sterile components, which requires sterilizing processes and may require extensive end-preparation testing depending on the BUD and volume produced.22
COMPOUNDING OPHTHALMIC PREPARATIONS
According to the USP <797> chapter on sterile compounding, all ophthalmics, topical and injectable, are sterile preparations.24 There is a myth that ophthalmic preparations can be prepared in a non-sterile environment because they are no longer "sterile" once the patient opens the container and administers the first dose. Even though there have been numerous reports of microbial contamination of compounded ophthalmic medications resulting in injury, infection, or even loss of an eye, some practitioners still prepare them in nonsterile conditions, such as countertops in pharmacies, medication rooms, or at the patient's bedside.29-31 Ophthalmic preparations are often used to treat acute conditions and may be needed quickly. They are not considered emergent, life-threatening treatments, however, and should be prepared in a controlled, sterile environment. According to the proposed USP <800> chapter on hazardous compounding, if the drug or components in the compounded ophthalmic preparation are hazardous, the compounder may need to prepare it in a negative-pressure, ISO-7 room in a ISO-5 Class II biological safety cabinet or compounding aseptic containment isolator.32
Most compounded ophthalmic preparations are prepared using commercial sterile ingredients and usually are topical solutions or ocular injections. However, some compounded ophthalmic dosage forms are prepared from bulk APIs because of manufacturer backorders or the compounded medication is not commercially available. They may be prepared as a single unit for an individual patient, or prepared as a batch in multiple units for an individual patient or multiple patients.26
Compounders must follow current official USP <797> standards when compounding ophthalmic preparations; USP is expected to publish a revised <797> chapter in June 2019 with an effective date of December 2019, and a revised chapter <800> will take effect with the new <797>.24 These standards include the requirements for compounding personnel; environment and environmental monitoring; equipment; categories of sterile preparations; quality assurance; end-product testing; assigning BUDs; packaging, handling, and transport of compounded sterile preparations; use and storage; redispensing; patient education and monitoring; and adverse events reporting. Compounders should read, understand, and implement this chapter of the United States Pharmacopeia before preparing compounded sterile medications. In addition to the USP <797> standards, there are a few published guidelines that are specific for ophthalmic preparations.22,33,34
Compounding Practices for the Preparation of Ophthalmics
Dosage forms, such as ocular injections, are usually very concentrated due to the volume required. Mathematical calculations used to develop the formula should be double-checked to minimize error. Decimal errors during ophthalmics' preparation could significantly increase or decrease the required dose by several fold and cause injury to the eye.22
To improve accuracy in measuring sterile ingredients being withdrawn from vials or bags, use the smallest syringe necessary to measure the desired volume. For example, use a 3 mL syringe to measure a 2.5 mL quantity rather than a 5 mL syringe. The 5 mL syringe has 0.2 mL increments on it, whereas the 3 mL syringe has 0.1 mL increments. When using liquid from a glass ampule in an ophthalmic, filter it through a 5-µm filter when removing liquid from the ampule to remove any particulate matter, such as glass shards from opening the ampule. Although not required, sterile powders for injection that have been reconstituted should also be filtered, if possible, through a 5-µm filter to remove particulate matter, such as a core from the vial stopper.34
Quality assurance is important in ophthalmic dosage forms' preparation. Compounders must inspect all ophthalmic dosage forms visually for clarity and particulate matter. Suspensions must be easily suspended when shaken, with no caking on the bottom. Ointments must be smooth, not grainy. The color must be as expected for that particular formulation. The final volume and weight should be as calculated and not vary more than 10% from the theoretical volume or weight. Finally, the compounder should check the pH to ensure that the solution is within a range suitable for the active ingredient(s) and the eye itself.22,26
Although a compounded ophthalmic preparation for an individual patient does not need to be tested, batch-prepared ophthalmic dosage forms for multiple patients must undergo a quarantine period and end-preparation testing. The USP <797> specifies that a batch of more than 25 units must be sterility tested. This is a minimum standard. Sterility testing any batch that affects multiple patients or has several doses for an individual patient is prudent and must be done according to the USP <797> standard. Certain ophthalmic preparations can be easily contaminated and support fungal growth.36
The USP <797> standard does not require endotoxin or potency testing for ophthalmic preparations; however, these tests may be appropriate for certain ophthalmic dosage forms. Typically, endotoxins are known for causing fever and other complications when injected into the bloodstream. There have been reported cases of ocular injections contaminated with endotoxins causing toxic anterior segment syndrome, which is an acute inflammation of the eye's anterior segment that usually occurs following cataract surgery. Potency testing should be done initially with the development of a new formula to ensure that the concentration of active medication and the process to prepare the dosage form is accurate.24
Another consideration for compounding ophthalmic preparations is container choice. For preservative-free preparations, it would be prudent to package the preparation in single-dose sterile bottles or syringes. For preparations that have short BUDs when stored at room temperature or refrigerated, the compounder may need to package the preparation in single-dose containers and instruct the patient, caregiver, or practitioner to freeze them and only thaw a 1-day or 2-day supply at any given time to extend the batch's BUD.26
SUMMARY
Although most ophthalmic dosage forms are relatively easy to prepare, several factors need to be considered when choosing to compound them:
- Target location of the eye requiring treatment
- Composition of the ophthalmic dosage form
- Requirements for the preparation of ophthalmic dosage forms
The compounder must also assess, according to the USP <797> standards and hazardous compounding guidelines or local, state and federal regulations, whether the environment or equipment is suitable to safely compound sterile and/or hazardous ophthalmic preparations. Properly preparing compounded ophthalmic dosage forms is essential in providing good quality preparations to effectively treat a delicate organ, the eye.
For more information on ophthalmic compounding, consult the review articles by Allen on basics of sterile compounding37 and suspensions/ointments.38
REFERENCES
- Hopkins G, Pearson R. Ophthalmic Drugs—Diagnostic and Therapeutic Uses. 5th ed. London, UK: Elsevier; 2007.
- Eye Health Topics. National Eye Institute, National Institutes of Health. July 10, 2015. Accessed at https://nei.nih.gov/, June 21, 2016.
- Venkata Ratnam B, Madhavi S, Rajesh P. Ocular drug delivery: an update review. Int J Pharm Bio Sci. 2011;1(4):437-446.
- Gaudana R. Ananthula HK, Parenky A. Mitra AK. Ocular drug delivery. AAPSJ. 2010;12(3):348-360.
- Baranowski P, Karolewicz B, Gajda M, et al. Ophthalmic drug dosage forms: characterisation and research methods. Sci World J. 2014:861904.
- Hanna C, Fraunfelder FT, Cable M, et all. The effect of ophthalmic ointments on corneal wound healing. Am J Ophthal. 1973;76(2):193-200.
- Summers A. Treating burns caused by hydrofluoric acid. Emerg Nurse. 2011;19(3):12-15.
- Plister RR. Chemical corneal burns. Int Ophthalmol Clin. 1984;24(2):157-168.
- Accordino A, Chambers RA, Thompson BC. The stability of a topical solution of cocaine hydrochloride. Austral J Hosp Pharm. 1996;26(6):629-633.
- Kallio H, Paloheimo M, Maunuksela E-L. Hyaluronidase as an adjuvant in bupivacaine-lidocaine mixture for retrobulbar/perbulbar block. Anesth Analg. 2000;91(4):934-937.
- Pucci N, Novembre E, Cianferoni A, et al. Efficacy and safety of cyclosporine eye drops in vernal kertoconjunctivitis. Ann Allergy Asthma Immunol. 2002;89(3):298-303.
- Wang Y, Ogawa Y, Dogru M, et al.Ocular surface and tear functions after topical cyclosporine treatment in dry eye patients with chronic graft-versus-host disease. Bone Marrow Transplant. 2008;41(3):293-302.
- Restasis [package insert]. Irvine, CA: Allergan;2013.
- McElhiney LF. Developing an erythromycin ophthalmic ointment – putting the puzzle pieces together. Int J Pharm Compound. 2010;14(4):270-274.
- Allen LV Jr. Rose bengal 1% ophthalmic solution. Int J Pharm Compound. 1998;2(3):231.
- MillodotM. Dictionary of Optometry and Visual Science. 7th ed. Edinburgh: Elsevier-Butterworth-Heinemann; 2009.
- Pickrell A, Harris A, Ngo S, et al. Delivery of intraocular triamcinolone acetate in the treatment of macular edema. Pharmaceutics.2012;4(1):230-242.
- Canavan KS, Dark A, Garrioch MA. Sub-Tenon's administration of local anaesthetics: a review of technique. Br J Anaesth.2003;90(6):787-793.
- Goldman DA. Intracameral therapy: the next step in management of ocular disease? September 19, 2008. Accessed at http://www.ophthalmologyweb.com/Featured-Articles/20009-Intracameral-therapy-The-next-step-in-management-of-ocular-disease/, June 22, 2016.
- Myers L, Almeida D, Abramoff MD. Intravitreal injection technique: a primer for ophthalmology residents and fellows. January 6, 2015. Accessed at www.eyerounds.org/tutorials/intravitreal-injection/, June 22, 2016.
- Peyman GA, Lad EM, Moshfeghi DM. Intravitreal injection of therapeutic agents. Retina. 2009;29(7):875-912.
- McElhiney LF. Compounding Guide for Ophthalmic Preparations. Washington, DC: American Pharmacists Association; 2013.
- Kibbe AH. Handbook of Pharmaceutical Excipients. 3rd ed. Washington, DC: American Pharmaceutical Association; 2000.
- United States Pharmacopeial Convention. USP General Chapter <797> Pharmaceutical Compounding—Sterile Preparations. In: United States Pharmacopeia 38/National Formulary 33. Rockville, MD: United States Pharmacopeial Convention; 2015.
- Trissel LA. Trissel's Stability of Compounded Preparations. 4th ed. Washington, DC: American Pharmacists Association; 2009.
- Allen Loyd V Jr. Chapter 21: Ophthalmic, Otic, and Nasal Preparations. In: The Art, Science, and Technology of Pharmaceutical Compounding. 4th edition. Washington, DC: American Pharmacists Association; 2012:307-330.
- Chedru-Legros V, fines-Guyon M, Cherel A, et al. In vitro stability of fortified ophthalmic antibiotics stored at -20°C for 6 months. Cornea. 2010;29(7):807-811.
- United States Pharmacopeial Convention. USP monographs: bland lubricating ophthalmic ointment. In: U.S. Pharmacopeia 34/National Formulary 29. Rockville, MD: United States Phamacopeial Convention; 2011.
- U.S. Food and Drug Administration. FDA alerts health care professionals of infection risk from repackaged Avastin intravitreal injections. Accessed at http://web.archive.org/web/20110901180651/http://www.fda.gov/Drugs/DrugSafety/ucm270296.htm. June 22, 2018.
- Associated Press. Eye injuries linked to contaminated drug. New York Times. November 10, 1990. Accessed at http://www.nytimes.com/1990/11/10/us/eye-injuries-linked-to-contaminated-drug.html, June 22, 2016.
- Centers for Disease Control and Prevention. Outbreaks of postoperative bacterial endophthalmitis caused by intrinsically contaminated ophthalmic solutions-Thailand, 1992, and Canada, 1993. MMWR Morb Mortal Wkly Rep. 1996;45(23):491-494.
- United States Pharmacopeial Convention. USP General Chapter <800> Hazardous Drugs—Handling in Healthcare Settings. December 1, 2014. Accessed at http://www.usp.org/usp-nf/notices/general-chapter-hazardous-drugs-handling-healthcare-settings, June 22, 2016.
- ASHP technical assistance bulletin on pharmacy-prepared ophthalmic products. Am J Hosp Pharm.1993;50(7):1462-1463.
- Reynolds LA, Closson RG. Extemporaneous Ophthalmic Preparations. Vancouver, WA: Applied Therapeutics; 1993.
- U.S. Food and Drug Administration. Recall of brilliant blue G urgent product recall—immediate action required. March 9, 2012. Accessed at http://web.archive.org/web/20120318172103/http://www.fda.gov:80/Safety/Recalls/ucm296326.htm, June 27, 2018.
- American Society of Cataract and Refractive Surgery, American Society of Ophthalmic Registered Nurses. Recommended practices for cleaning and sterilizing intraocular surgical instruments. J Cataract Refract Surg. 2007;33:1095-1100.
- Allen LV Jr. Basics of sterile compounding: ophthalmic preparations, part 1: ophthalmic solutions. Int J Pharm Compd. 2016(Sep-Oct);20(5):399-404.
- Allen LV Jr. Basics of sterile compounding: ophthalmic preparations, part 2: suspensions and ointments. Int J Pharm Compd. 2016(Nov-Dec);20(6):495-500.
Back to Top