ADVERTISEMENT

Optimizing Care of Patients with Heart Failure-Article
Optimizing care in patients with heart failure is essential if we want patients to feel better, prevent hospitalizations, and decrease mortality. Optimizing care means not only optimizing guideline-directed medical therapy (GDMT) but also addressing comorbidities, adherence, barriers to adherence, and patient self-management. This article will provide key concepts and approaches to further optimize patient care in HF in conjunction with GDMT.
Guideline-Directed Medical Therapy (GDMT)
Extensive review of GDMT can be found elsewhere.1-3 This article will highlight key concepts for recommended drug classes and patient counseling points. When evaluating patients for GDMT, overall, there are a number of key concepts to consider:
- All patients with HF and reduced ejection fraction (HFrEF) should be considered for therapy with an angiotensin converting enzyme (ACE) inhibitor, angiotensin receptor blocker (ARB) or angiotensin receptor/neprilysin inhibitor (ARNI) (ACE/ARB/ARNI); beta blocker (BB); and aldosterone antagonist (AA) to reduce morbidity and mortality.
- For patients who tolerate ACE/ARB, consideration should be made to switch to ARNI.
- Titrate patients to target doses if appropriate.
- Being on lower doses of multiple rather than a high dose of a single GDMT is preferred.
- Patients should be evaluated for other therapies including ivabradine, hydralazine and isosorbide dinitrate, digoxin, and omega-3 polyunsaturated fatty acid (PUFA) where appropriate.
- Talk to your patients, to emphasize the importance of GDMT therapy in regard to symptoms, hospitalizations, and mortality.
Diuretics
Key concepts for the use of diuretics in HF are outlined in Table 1. An important concept for loop diuretics is that the diuretic threshold needs to be reached. As shown in Figure 1, loop diuretics have a steep dose-response curve. In order to reach a significant diuresis, urinary concentrations of diuretic need to reach the upper portion of the curve. Clinically, this means that high doses of diuretics may be needed to induce diuresis, especially in patients with poor renal function.
Table 1. Key Concepts: Diuretic Therapy
Key Concepts
- Evaluate for symptom relief (e.g., shortness of breath, orthopnea)
- Evaluate weight and signs of fluid retention (e.g., edema)
- Urine output. In the ambulatory setting talk to patients, ask what happens after they take their diuretic. If there is no increase in urine output within a 1- or 2-hour period, therapy may need to be modified.
- Monitor electrolyte levels, in particular, hypokalemia, hypomagnesemia, and hyponatremia.
- Monitor blood pressure. If patients experience hypotension, evaluate for dehydration.
- Monitor renal function. Diuretics may increase serum creatinine levels, especially with aggressive therapy. Increase in serum creatinine levels may also be seen in patients who become dehydrated.
- Monitor for hyperuricemia/gout.
- All loop diuretics are equally effective at equivalent doses.
Patient Counseling
- Explain expected benefits: decrease shortness of breath and edema (or other patient-specific symptoms associated with fluid overload)
- Expect increased urination. In most cases take in morning versus at bedtime.
- Patients need to self-monitor: urine output, weight gain (>2lbs), shortness of breath and edema.
- In case of significant increase in signs and symptoms of fluid overload, patient should be instructed to call their health care provider.
- Report dizziness (evaluate for dehydration and hypotension)
- Avoid NSAIDs, which may decrease diuretic effects and may cause renal impairment.
|
Figure 1. Pharmacodynamics of Loop Diuretics
 |
| Adapted from: Brater DC. Pharmacology of diuretics. Am J Med Sci. 2000;319:38-50. |
Perhaps the most important assessment for diuretic therapy is to ask the patient what happens after they take their diuretic. If there is a change in response or if urine output is not increased over a 6-hour period (usually 1 or 2 hours), patients need be evaluated for "diuretic resistance." The appearance of diuretic resistance can be attributed to a number of factors. One factor to consider is the dose of the loop diuretic. As mentioned, patients need to achieve the diuretic threshold to achieve a good response. This concept is especially important in patients on low doses of loop diuretics, for whom increasing the dose (e.g., doubling dose of furosemide) should be a consideration.
Another factor to consider is medication and dietary adherence. Patients who are not taking their loop diuretic will have fluid retention which may lead to an assumption that the patient is resistant to the diuretic. In fact, if they were adherent, symptoms of fluid retention would not be apparent. Patients who are not adherent with dietary restrictions (e.g., sodium intake) may have symptoms and still have a good diuretic response. For example, if a patient increases sodium intake, a single daily dose of diuretic cannot sufficiently excrete the excess sodium, so fluid retention occurs. For patients who are not adherent to their dietary restrictions increasing the frequency of dosing (assuming the dose is at the patient's diuretic threshold) can manage the excess fluid on a short-term basis.
A third factor to consider is a change in absorption that may occur, especially with furosemide, when patients begin to decompensate. Specifically, as the gut becomes edematous there is delayed absorption resulting in a decrease in Cmax. If this occurs, the diuretic threshold will not be reached. In these cases, the diuretic dosage needs to be increased or the patient needs to be switched from furosemide to a diuretic with better bioavailability and more consistent absorption, such as torsemide.4
Another consideration for decreased diuretic effectiveness is drug interactions, especially with nonsteroidal anti-inflammatory drugs (NSAIDs), which can lead to decreased renal function and sodium retention. The final consideration is the induction of distal tubular hypertrophy, which may occur in patients receiving chronic therapy with loop diuretics. It is hypothesized that cells in the distal tubular section in response to seeing high levels of urinary sodium caused by the administration of loop diuretics will hypertrophy. These enlarged cells become more efficient in reabsorbing sodium such that the effects of loop diuretics in blocking sodium reabsorption in the loop of Henle is negated by enhanced reabsorption of sodium in the distal segment. To overcome the effects of distal tubular hypertrophy a combination of a loop diuretic and a thiazide-type diuretic is recommended to increase urinary output. The effect of a thiazide diuretic to increase diuretic responsiveness appears to be a class effect. Hydrochlorothiazide (usual dose range 25 to 100 mg once or twice daily) and metolazone (usual dose range 2.5 mg to 10 mg once daily) are thiazide diuretics commonly used in combination with loop diuretics. Hydrochlorothiazide and metolazone differ in duration of action; the long duration of action of metolazone may make it more effective than hydrochlorothiazide in some patients. However, if patient is over-diuresed then the longer duration of action for metolazone may become detrimental. Key concepts for overcoming diuretic resistance are outlined in Table 2.
Table 2. Key Concepts for Overcoming "Diuretic Resistance"
- Improve drug and dietary compliance
- Discontinue interacting drugs (e.g., NSAIDs)
- Make sure drug is administered at threshold dose
- Increase dose if not at threshold
- Increase frequency if at threshold (bid – tid dosing)
- ↓ absorption? – change to torsemide or bumetanide
- Add thiazide-type diuretic if distal tubular hypertrophy is suspected.
|
The pharmacist's role in optimizing medication therapy in HF includes managing the dosage and potential contraindications or drug interactions of GDMT, as well as counseling patients about these therapies in order to maximize their adherence and benefits of treatment. Key concepts for medication management and patient counseling for the various medication categories used in HF are discussed in Tables 3 – 7.
Table 3. Key Concepts: Use of ACE Inhibitors, ARBs, and ARNI in Heart Failure
- Cough with ACE inhibitor therapy is usually a dry cough and can take from weeks to months to occur. In some patients the cough may resolve on its own with continued therapy but may take months for spontaneous resolution. If the cough is persistent and bothersome, patient can be switched to ARB. If the ACE inhibitor is discontinued, resolution of the cough may take anywhere from 1 to 12 weeks.
- Increase in serum creatinine may be seen upon initiation or up-titration, especially in patients who are not clinically stable, are dehydrated, or develop hypotension upon initiation. The increase in serum creatinine is often minor and transient and may return to baseline over time. A chronic increase in serum creatinine, if limited, is acceptable. (Evaluate other drugs that may affect kidney function, discontinue if appropriate). May need to reduce dose or discontinue therapy if function is moderately or severely compromised.
- Renal impairment is not a contraindication to therapy. Patients with serum creatinine > 2mg/dL can be started on medication – need to monitor renal function and potassium levels closely.
- Sacubitril/valsartan should not be administered together with ACE inhibitors.
- In patients receiving sacubitril/valsartan and measuring natriuretic peptides for HF management need to measure NT-pro BNP. BNP levels will be elevated following sacubitril/valsartan therapy due to inhibition of neprilysin.
Patient Counseling
- Expected benefits: improved symptoms, decreased hospitalizations, increased survival
- Report symptoms of dizziness, cough
- Avoid NSAIDs, which may decrease diuretic effectiveness and decrease renal function.
- Serious allergic reactions causing swelling of face, lips, tongue, and throat (angioedema) may lead to trouble breathing and death. Get emergency medical help right away
- Do not take sacubitril/valsartan for at least 36 hours before or after you take an ACE inhibitor medicine.5
|
Table 4. Key Concepts: Beta-Blocker Therapy
- Start low (bisoprolol 1.25 mg qd, carvedilol 3.125 mg bid, metoprolol succinate 12.5 to 25 mg qd).
- Patients need to be clinical stable and euvolemic before starting or increasing dose.
- Titrate upward no sooner than every 2 weeks and often in clinical practice patients are up-titrated over a time period of months.
- In some patients, upon initiation or increase in dose, HF symptoms (dyspnea, fatigue, edema) may get worse. These symptoms are often transient and can be managed by increasing diuretic dose or frequency. If symptoms are persistent may need to reduce dose or discontinue beta-blocker therapy.
- Symptom improvement may take months.
- Asthma is a relative contraindication. Consider cardio-selective beta-blocker such as bisoprolol or metoprolol succinate.
- For patients with COPD, consider cardio-selective beta -locker such as bisoprolol or metoprolol succinate.
- Metoprolol succinate should be prescribed, not metoprolol tartrate.
Patient Counseling
- Expected benefits: improve symptoms, decrease hospitalizations, increase survival.
- Symptom improvement may take months (3 to 6 months)
- May feel worse before feeling better (upon dose initiation or during up titration).
- Report worsening symptoms including weight gain. These symptoms can be managed but patient NEEDS to stay on therapy! (Reinforce importance of beta-blocker therapy to the patient).
- Do not stop taking beta-blocker unless directed by physician.
|
Table 5. Aldosterone Antagonists
Key Concepts
- To initiate: Creatinine should be 2.5 mg/dL or less in men or 2.0 mg/dL or less in women (or estimated glomerular filtration rate >30 mL/min/1.73m2) and potassium should be less than 5.0 mEq/L.1
- Electrolytes (K+) should be checked upon initiation and re-checked within 2 to 3 days and again after 7 days.1
- Additional monitoring will be patient-dependent but should occur at least monthly for the first 3 months and every 3 months afterwards or sooner if warranted.
- Reevaluate need for potassium supplements and consider discontinuing. Of note, salt substitutes contain potassium. Also consider dietary evaluation if potassium levels are elevated.
- Increase in serum creatinine may occur. Can be associated with increase diuresis seen with aldosterone antagonists. May need to reduce loop diuretic therapy. Serum creatinine increase may be transient – monitor over time.
- Discontinue drugs that may affect the kidney (e.g., NSAIDs) if potassium or serum creatinine levels increase.
- In patients who develop significant hyperkalemia (usually > 5.5 mEq/L but may be patient dependent) requiring discontinuation of therapy, consider using an oral potassium binder.
Patient Counseling
- Expected benefits: improved symptoms, decreased hospitalizations, increased survival.
- Expect increased urination.
- Report dizziness (evaluate for dehydration and hypotension).
- Avoid NSAIDs, which may decrease diuretic effectiveness and decrease renal function.
|
Table 6. Hydralazine and Isosorbide Dinitrate
Key Concepts
- Avoid volume depletion when starting hydralazine and isosorbide dinitrate to help prevent hypotension
- Start low doses to help avoid headaches associated with nitrate therapy.
- Use of a mononitrate agent is not recommended in the guidelines. Clinically, patients may be prescribed mononitrate therapy, but outcomes using an agent other than isosorbide dinitrate (single or in combination product) are unknown. Guidelines do not recognize a class effect for nitrates.
Patient Counseling
- Expected benefits: improved symptoms, decreased hospitalizations, increased survival.
- Advise patients that headaches are common with this medication, especially when starting or changing dose. Over time, headaches may lessen.
- Report dizziness or lightheadedness upon standing.
- Warn patients not to take phosphodiesterase-5 inhibitors (e.g., sildenafil, vardenafil, or tadalafil) due to severe and possibly life-threatening drug interaction.
- Report symptoms such as arthralgia, fever, malaise and other signs that may relate to systemic lupus erythematosus.
|
Table 7. Ivabradine for Heart-Rate Lowering in HF6
Key Concepts
- Ivabradine dose should be reduced if the resting heart rate is persistently below 50 beats per minute or it patient experiences symptoms of bradycardia (hypotension, dizziness, fatigue, shortness of breath). Evaluate for drug interactions that may interfere with ivabradine metabolism and re-evaluate need for other heart-rate lowering drugs if appropriate.
- Ivabradine should be stopped if atrial fibrillation develops during therapy.
- Luminous phosphenes may occur, generally within the first 2 months. Approximately 15% of patients receiving the highest dose (10 mg bid) and 2% of patients receiving the 5 and 2.5 mg doses may experience this adverse effect. However, fewer than 1% of patients discontinue therapy. Luminous phophenes are often described as enhanced brightness in limited areas of the visual field (spots). This phenomenon can also be described as a halo and colored bright lights. Luminous phosphenes may resolve during therapy or after stopping treatment.
Patient Counseling
- Expected benefit: reduces risk of HF hospitalization
- Patients should take ivabradine with meals.
- Patients should not ingest either grapefruit juice or St John's wort while taking ivabradine.
- Discuss with patients the potential risk of luminous phenomena. Patients should be advised to use caution if they are driving or using machines in situations where sudden changes in light intensity may occur, such as driving at night.
- Advise patients to report dizziness, fatigue, or shortness of breath to their health care professional.
- If appropriate, teach patients how to monitor their pulse and to report when resting heart rate is < 50 beats/minute.
|
Management of Common Comorbidities
Diabetes
Diabetes is associated with higher hospitalization and mortality rates in patients with HF. The findings are consistent and have been shown in secondary analyses of a number of large HF trials.8,9 Patients with HF and diabetes should be treated with GDMT for heart failure and will derive benefits similar to those in patients who do not have diabetes. For patients with type 1 diabetes, insulin is required. Insulin administration may cause sodium retention in some cases and may require adjustment in the diuretic dose. For patients with type 2 diabetes, initial consideration for therapy should include metformin.10 Previous meta-analyses have shown that metformin is associated with a reduction in mortality and cardiovascular mortality compared to sulfonylurea therapy.11,12
A recent meta-analysis evaluated the clinical outcomes associated with metformin in populations for whom metformin is typically contraindicated (chronic kidney disease, congestive heart failure, or chronic liver disease).13 The results showed that metformin use was associated with reduced all-cause mortality and fewer hospital admissions for HF. A historical concern with metformin has been the potential for patients to develop lactic acidosis. Based on this, HF was once considered a contraindication to the use of metformin. Today, caution is recommended for the use of metformin mainly in acute or unstable HF. Another meta-analysis indicated no clear association between metformin administration and the development of lactic acidosis.14 Recently, the FDA has revised its warning regarding renal function and the use of metformin and has moved from creatinine to eGFR definition. Specifically, metformin is contraindicated in patients with an eGFR below 30 mL/minute/1.73m2. This less-stringent definition increases the number of patients who may benefit from the use of metformin. Current American Diabetes Association (ADA) guidelines should be followed with regard to targeted HbA1c levels.10 For HF patients the target would most likely range from <7% up to <8% in higher-risk patients.
In regard to combination therapy, recent data suggest that empagliflozin, a sodium-glucose cotransporter-2 inhibitor, should be considered for initial add-on therapy. Empagliflozin was recently studied in approximately 7,000 patients with type 2 diabetes with the primary outcome of cardiovascular death, non-fatal MI, and non-fatal stroke.15 The results demonstrated a significant 14% reduction in the primary endpoint (P = 0.04) and a 35% reduction in HF admissions (P = 0.002) in a secondary analysis. The results of this study led to empagliflozin's current indication for lowering HbA1c levels and reducing the risk of cardiovascular death in adult patients with type 2 diabetes mellitus and established cardiovascular disease.16 Of particular note with the use of empagliflozin is that patients may experience a diuretic-type effect and effects on blood pressure. Add-on therapies associated with worsening heart failure should be avoided, including thiazolidinediones along with saxagliptin and sitagliptin. For additional recommendations for add-on or combination therapies in patients with diabetes, refer to the American Diabetes Association (ADA) guidelines.10
Depression
Approximately 21% (9% to 60%) of HF patients may have depression. Depression in HF patients can led to poor quality of life, limited functional status, and increased morbidity and mortality. In addition, depression can led to poor self-care. Screening of patients with HF for depression should be considered in the clinic or pharmacy setting. For initial screening simple assessment tools can be administered by the pharmacist in a time-efficient manner, including the Patient Health Questionnaire – 2 and – 9.17 Heart failure guidelines do not provide clear guidance for the treatment of depression. The SADHART-CHF study evaluated the role of sertraline compared to placebo for the treatment of depression in 469 HF patients for 12 weeks.18 The results showed minimal effects but drug therapy appeared to be safe. In part, the lack of response to sertraline in the short term may relate to the effectiveness of nurse-facilitated supportive intervention which was part of the study and was provided to the placebo group. In the MOOD-HF trial, escitalopram was compared to placebo in 327 patients and demonstrated no effect on hospitalizations or mortality and no improvement in symptoms of depression.19 Up to this point, treatment of HF patients with antidepressants has been disappointing. Sertraline and escitalopram, both serotonin reuptake inhibitors (SSRIs), appear to be safe to use in HF patients. Other antidepressants, especially tricyclic antidepressants, should be avoided in HF patients given their many cardiovascular side effects—including QTc prolongation, orthostatic hypotension, and anticholinergic effects. Caution should be exercised when using antidepressants that may affect drug metabolism enzymes. In particular, both fluoxetine and paroxetine are strong CYP2D inhibitors and may significantly affect the metabolism of carvedilol and metoprolol, leading to higher serum concentrations and greater beta-blocking effects.20,21 St. John's wort should also be avoided due to potential drug interactions. Other therapies to consider for managing depression in patients with HF include counseling and exercises such as Tai-Chi and yoga.
Hyperkalemia
Therapeutic interventions that improve morbidity and mortality include blockers of the renin-angiotensin-aldosterone system (RAAS). Therapeutic classes of RAAS inhibitors include ACE inhibitors, ARBs, ARNI, and aldosterone antagonists. Inhibiting RAAS can lead to potassium retention and potentially hyperkalemia. HF patients at particular risk for developing hyperkalemia include those with renal dysfunction and diabetes. If hyperkalemia develops patients may need to discontinue life-saving medications such as ACE inhibitors and aldosterone antagonists. Recently, a new non-absorbed potassium binder, patiromer (Veltassa), has been approved for the treatment of hyperkalemia. Before the approval of patiromer, the only available potassium binding resin available for maintenance therapy was sodium polystyrene sulfonate. The use of this resin has been limited secondary to fluid retention and severe gastrointestinal complications including colonic necrosis. Patiromer has been shown to be effective in reducing potassium levels in patients with chronic kidney disease, diabetes, and HF.22-24 Most adverse effects observed in the trials were mild and included gastrointestinal symptoms (constipation, diarrhea, nausea, abdominal discomfort) and hypomagnesemia. Drug interactions are a concern with patiromer and it is recommended that patients take other orally administered drugs at least 3 hours before or 3 hours after patiromer administration.25 For those patients who are unable to tolerate RAAS inhibitors secondary to development of hyperkalemia, patiromer may be an attractive option. Another potassium binder that is currently being evaluated by the FDA is sodium zirconium cyclosilicate (ZS-9) which, if approved, will provide another option for treating hyperkalemia. Treatment of drug-induced hyperkalemia in HF patients is promising given the new generation of potassium binders. Studies evaluating chronic therapy in preventing hyperkalemia and optimizing RAAS inhibitor therapy are needed.
Self-Care, Over-The-Counter (OTC) Medications, and Adherence
The use of OTC medications by HF patients is reported to be high ( >60%). OTC medications are used to treat mainly, pain, cough and cold, and gastrointestinal symptoms. Key concepts for managing OTC medication use among HF patients for treatment of pain, cough and cold, and GI symptoms are outlined in Table 8.
Table 8. Managing OTC Medication Use in HF
Key Concepts – General Pain Management
- Avoid NSAIDs and corticosteroids if possible may cause fluid retention and worsening renal function with NSAIDs
- Consider use of acetaminophen, topical methyl-salicylate products (general pain), topical capsaicin (OA, joint pain), topical NSAIDs (osteoarthritis, joint pain)
- Consider tramadol (use caution in patient with impairment of renal function)
- Consider opiates
- Consider chondroitin sulfate and glucosamine for joint pain (caution, may have interaction with warfarin)
- Consider non-pharmacologic approaches such as exercise, acupuncture, Tai-Chi
- Evaluate for statin-induced muscle pain in appropriate patients
Key Concepts – Cough and Cold Management
- Most cases avoid sympathomimetic decongestants (e.g. pseudoephedrine, phenylephrine)
- Consider antihistamines (avoid diphenhydramine – prolong QTc interval)
- Consider use of dextromethorphan
- Consider the use of nasal saline wash
- Caution with the use of nasal sympathomimetics (prolong or excessive use can lead to cardiovascular complications)
- Consider the use of zinc cold products to reduce duration of symptoms
- Evaluate sodium content of liquid preparations
Key Concepts – Antacids and Laxatives
- Antacids
- Evaluate for sodium content
- Evaluate for magnesium content especially in patients with impaired renal function
- Excess magnesium intake can lead to hypermagnesemia in HF patients with impaired renal function
- Evaluate for drug-drug interactions26
- Laxatives
- Monitor for dehydration and electrolyte disturbances
- Bulk forming laxatives evaluate for drug interactions
- Hyperosmotic saline laxatives (e.g. magnesium citrate) evaluate for hypermagnesemia
|
Medication Adherence
A key concept to improving outcomes in patients with HF is medication adherence. Medication nonadherence ranges from 40% to 60% and may contribute to approximately 30% of hospital admissions. In addition, medication nonadherence is associated with increased cardiac-related events, increased health care costs, and reduced quality of life. Methods for assessing medication adherence include self-report (ask the patient), pill counts, drug levels, and refill rates. In addition medication adherence tools can be used, such as the Morisky-4, Adherence Estimator.27,2
Unfortunately, nonadherence is often associated with multiple barriers. When talking to patients, the pharmacist should explore adherence barriers and work with patients to create solutions. Barriers to medication adherence may include: complex medication schedule; use of multiple drugs; drug cost; transportation; lack of family support; health beliefs; health literacy; and cognitive impairment. Often the approach to improving medication adherence is multifactorial. However, at times it can be very simple, such as providing a way to help patients remember to take their medications. This may be as simple as a "pill box" or the use of technologies such as smart phones for appropriate patients. A recent survey in 100 HF patients demonstrated that 85% of patients had internet access and over 40% used a smart device and were confident in its use, accessing their smart device >10 times/day.29 In these patients, using health "apps" may help improve medication adherence, self-care, and therapeutic life style. For example, there are over 200 medication adherence apps, and over 1,000 diet and personal fitness apps. A recent study evaluated and rated a number of medication adherence applications.30 Guiding patients in the use of these technologies may present another opportunity for the pharmacist to help patients improve their health care.
Clinical Assessment Tools
Cognitive Function
Cognitive impairment can lead to increased hospitalizations, mortality, and health care costs in patients with HF. The incidence of cognitive impairment ranges from 25% to 75% in patients with HF (90% in patients with hyponatremia).31 Cognitive impairment can be seen in young and older patients and in HF patients with and without reduced ejection fraction. Every HF patient should be assessed for cognitive impairment since it may significantly affect the patient's ability to engage in self-care and adhere to medication regimens. Assessing cognitive function can be done quickly and efficiently by the pharmacist using a tools such as the Mini-Cog and the Montreal Cognitive Assessment.32,33
Heart Failure Assessment
Pharmacists, especially in the community setting, can and should assess patients for sign and symptoms of worsening HF. These assessments can be done in a timely and efficient manner by the pharmacist, pharmacist technician, or pharmacy student using a published clinical tool, TOM-CHF.34,35 Importantly, if worsening symptoms are seen, real-time interventions can be made which may prevent hospitalization. Previous studies in this area have shown that community pharmacists can detect worsening HF in patients in the community setting. For example, of the 121 self-identified HF patients assessed in 10 community pharmacy settings, 62% of patients had signs or symptoms of worsening HF which included increased edema and shortness of breath.34 In another study, pharmacy students were able to drive the assessment process and recommend interventions for the patient in real time (e.g., change diuretic dose, frequency, and up-titration of GDMT).35 Heart failure assessment by pharmacists can be accomplished in the community, clinic, and long term care settings. In expanding pharmacy-based clinical service (assessments), pharmacists can help patients better manage their HF.
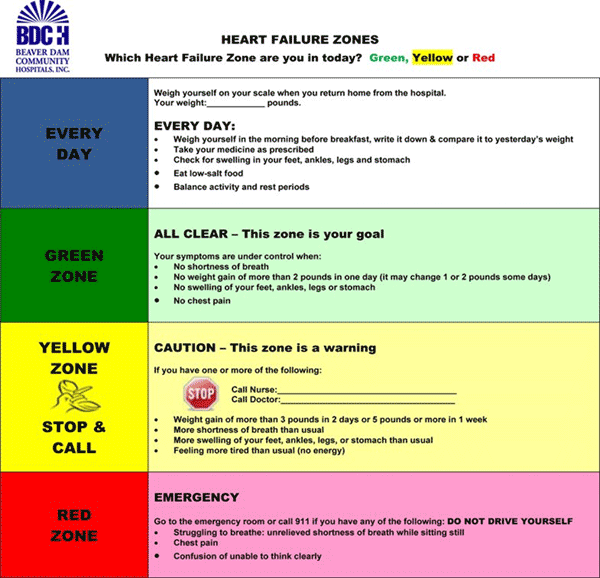
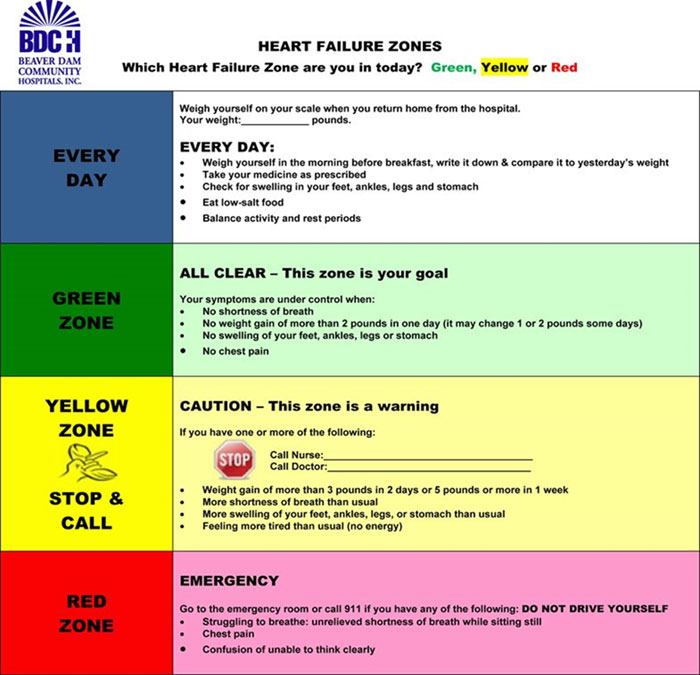
Self-Management
Perhaps the most important way to improve outcomes including decreased hospitalizations and improved quality of life is to encourage patients to be involved with their care. Patient self-management needs to be reinforced and where possible barriers to self-management should be addressed (Table 9). A key concept to improve patient self-management is knowledge about their condition. There are a number of resources and tools available to help patients better understand and monitor their symptoms and overall condition (Figure 2).36 For example, the American Heart Association (AHA) provides extensive information for patients with HF on its website. For professionals there are also resources for patient education materials provided through the Get With The Guidelines®-Heart Failure program.37 In addition to AHA, both the American College of Cardiology (CardioSmart program) and Heart Failure Society of America (HFSA) have resources for patients and health care professionals. HFSA also offers a free mobile app to download to help patients manage their medications and track symptoms.
Table 9. Key Concepts in Promoting Patient Self-Care
Improving Medication Adherence
- Identity reasons for medication nonadherence
- Ask patients how they take their medication
- Involve family and caregivers
- Consider using motivational interviewing techniques
- Pill reminders, pill boxes, and medication adherence applications
- MTM review – may be able to reduce number of medications
- Keep it SIMPLE
- Simplify the regimen
- Impart knowledge
- Modify patient beliefs and behavior
- Provide communication and trust
- Leave the bias
- Evaluate adherence
Reinforcing Patient Self-Management
- Take medications as directed
- Follow dietary recommendations
- Check weight daily (log, mobile app) and take action right away when weight goes up
- Monitor for symptoms and take action right away when they occur
- Report dizziness or lack of diuretic effect
- Stay active
- See doctor and pharmacist regularly
- Seek social support
|
Figure 2. Example of a Simple Patient Tool for Self-Management36
Conclusion
Given the number of therapies HF patients need, it is essential that we optimize each individual therapy to the patient. We need to promote medication adherence and self-management and help patients overcome barriers to adherence. Importantly, we need to work with patients to help them understand their medications and their heart failure so that they can better take care of themselves.
REFERENCES
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;128:e240-e327.
- Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2016;37:2129-2200.
- Yancy CW, Jessup M, Bozkurt B, et al. 2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure. Circulation. 2016;134:e282-e293.3.
- Bleske BE, Welage LS, Kramer WG, Nicklas JM. Pharmacokinetics of torsemide in patients with decompensated and compensated congestive heart failure. J Clin Pharmacol. 1998;38:708-714.
- Entresto™ [package insert]. East Hanover, NJ: Novartis Pharmaceutical Corporation; 2015.
- Corlanor® [package insert]. Thousand Oaks, CA: Amgen Inc. 2017.
- Adams KF Jr, Patterson JH, Gattis WA, et al. Relationship of serum digoxin concentration to mortality and morbidity in women in the digitalis investigation group trial: a retrospective analysis. J Am Coll Cardiol. 2005 Aug 2;46:497-504.
- Gustafsson I, Brendorp B, Seiback M, et al. Influence of diabetes and diabetes-gender interaction on the risk of death in patients hospitalized with congestive heart failure. J Am Coll Cardiol. 2004;43:771-777.
- Nasir S, Aguilar D. Congestive heart failure and diabetes mellitus: Balancing glycemic control with heart failure improvement. Am J Cardiol. 2012;110[suppl]:50B–57B.
- American Diabetes Association. Standards of medical care in diabetes - 2017. Diabetes Care. 2017;40(Suppl. 1):S1–S134.
- Lamanna C, Monami M, Marchionni N, Mannucci E. Effect of metformin on cardiovascular events and mortality: a meta-analysis of randomized clinical trials. Diabetes Obes Metab. 2011;13:221-228.
- Boles S, Tseng E, Hutfless S, et al. Diabetes medications for adults with type 2 diabetes: An update. Comparative effectiveness review no. 173. Rockville: Agency for Healthcare Research and Quality; 2016.
- Crowley MJ, Diamantidis CJ, McDuffie JR, et al. Clinical outcomes of metformin use in populations with chronic kidney disease, congestive heart failure, or chronic liver disease. A systematic review. Ann Intern Med. 2017 Jan 3. doi: 10.7326/M16-1901. [Epub ahead of print]
- Salpeter SR, Greyber E, Pasternak GA, Salpeter EE. Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database Syst Rev. 2010:CD002967
- Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117-2128.
- Jardiance® [package insert] Boehringer Ingelheim Pharmaceuticals, Inc.; Ridgefield, CT; 2016.
- Patient Health Questionnaire (PHQ) Screeners. Available at: http://www.phqscreeners.com/.
- O'Connor CM, Jiang W, Kuchibhatla M, et al. SADHART-CHF Investigators. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J Am Coll Cardiol. 2010;56(9):692-699.
- Angermann CE, Gelbrich G, Stork S, et al. Effect of escitalopram on all-cause mortality and hospitalization in patients with heart failure and depression. The MOOD-HF Randomized Clinical Trial. JAMA. 2016;315(24):2683-2693.
- Stout SM, Nielsen J, Bleske BE, et al. The impact of paroxetine coadministration on stereospecific carvedilol pharmacokinetics. J Cardiovasc Pharmacol Ther. 2010;15(4):373-379.
- Stout SM, Nielsen J, Welage LS, et al. Influence of metoprolol dosage release formulation on the pharmacokinetic drug interaction with paroxetine. J Clin Pharmacol. 2011; 51(3):389-962.
- Weir MR, Bakris GL, Bushinsky DA, et al; for OPAL-HK Investigators. Patiromer in patients with kidney disease and hyperkalemia receiving RAAS inhibitors. N Engl J Med. 2015;372(3):211-22.
- Bakris GL, Pitt B, Weir MR, et al; for AMETHYST-DN Investigators. Effect of patiromer on serum potassium level in patients with hyperkalemia and diabetic kidney disease: the AMETHYST-DN randomized clinical trial. JAMA. 2015;314(2):151-161.
- Pitt B, Anker SD, Bushinsky DA, et al. Evaluation of the efficacy and safety of RLY5016, a polymeric potassium binder, in a double-blind, placebo-controlled study in patients with chronic heart failure (the PEARL-HF) trial. Eur Heart J. 2011;32(7):820-828.
- Veltassa® [package insert] Relypsa, Inc. Redwood City, CA; 2016..
- Ogawa R1, Echizen H. Clinically significant drug interactions with antacids: an update. Drugs. 2011;71:1839-64.
- Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67-74.
- Adherence Estimator. Available at: http://www.adherenceestimator.com/
- Dorsch MP, Chong YP, McCormick MP, et al. Survey of computer, smart devices, and Internet use in heart failure patients. International Cardiovascular Forum Journal. 2016;6:84-85.
- Dayer L, Heldenbrand S, Anderson P, et al. Smartphone medication adherence apps: potential benefits to patients and providers. J Am Pharm Assoc. 2013; 53:172-181.
- Albabtain M, Brenner J, Nicklas JM, et al. Hyponatremia, cognitive function, and mobility in an outpatient heart failure population. Med Sci Monit. 2016;22:4978-4985.
- http://mini-cog.com/mini-cog-instrument/standardized-mini-cog-instrument/
- MoCA Montreal - Cognitive Assessment. Available at: http://www.mocatest.org/
- Bleske BE, Dillman NO, Cornelius D, et al. Heart failure assessment as the community pharmacy level: a feasibility pilot study. J Am Pharm Assoc. 2014;54(6):634-41.
- Kelling SE, Walker PC, Mason JG, Bleske BE. Incorporation of a community pharmacy-based heart failure assessment tool by advanced pharmacy practice experience students. J Am Pharm Assoc. 2017. In press
- Agency for Healthcare Quality and Research (AHRQ). Red-Yellow-Green Congestive Heart Failure (CHF) Tool. Updated 2008. Available at: https://innovations.ahrq.gov/qualitytools/red-yellow-green-congestive-heart-failure-chf-tool.
- American Heart Association. Get With the Guidelines® – Heart Failure Clinical Tools. http://www.heart.org/HEARTORG/
Back to Top