
Expired activity
Please go to the PowerPak
homepage and select a course.
Module 9. Common Drugs that Affect Diabetes Control
Introduction
Even the most seasoned health care providers (HCPs) have found diabetes to be among the most
challenging diseases to manage. The difficulties arise from the dynamic nature of this disease
state, the lack of patient knowledge about the potential side effects of treatment, and the
relatively common practice of nonadherence. Type 2 diabetes mellitus (T2DM), in particular, is
progressive and, as the disease advances, patients are forced to evolve with it or risk long-term
adverse patient outcomes. Even when the appropriate therapy is chosen, there is still the
significant risk of medication side effects and interactions. Pharmacists are acutely attuned to the
risks of medication use; but, with dozens of possible medications and even more supplements,
sometimes choosing from this seemingly overwhelming sea of treatment options can be intimidating. The purpose of this module is to provide education to help you understand how
multiple medications in patients with diabetes can affect blood glucose (BG) metabolism.
Prescription-drug use among adults has risen substantially in the United States (U.S.) since 1999. In a 2013 report, the
most substantial increases in prescription-drug use were seen in patients 40 to 65 years of age
and those aged 65 years and older.1 The most commonly prescribed medications, not
surprisingly, were for hypertension, hyperlipidemia, diabetes, and depression. With so many new
interventions and so many drugs coming off patent, polypharmacy (i.e., a patient on 5 or more
clinically relevant agents) among those affected is now the new normal and it is part of the
pharmacist’s role as a HCP to ensure that the combination of medications does not lead to
negative outcomes.
There are multiple ways in which medications can impact diabetes control. Some medications
may alter BG test results, creating false high or low blood-sugar readings. The detriment in this
is obvious and could be quite serious. Other agents can cause substantial weight gain, leading to
greater insulin resistance and subsequently higher BG levels. Drug interactions that might make
the medications used for diabetes control more or less effective are also possible. The more
medications a patient takes, the more likely he or she is to experience drug interactions that could
cause harm. This point may seem intuitive, but it is something we should not forget or take
lightly. One study by Nolan and O’Malley suggested that senior patients who were taking 10 or
more medications had a 90%-plus probability of experiencing one or more drug interactions of
clinical significance.2 This percentage may seem alarming, but it reinforces the concept that
pharmacists must remain vigilant and well-educated while managing medication use, especially
for frail and older adult patients. Pharmacists are the last line of defense between physicians
trying to prescribe the right therapy and patients taking multiple agents that could interact and
potentially cause them harm.
The Physiology of BG Metabolism
The first step toward a better understanding of diabetes and the medications that might affect
control is to know the physiology of BG metabolism. This will allow for better recognition of the
effects medications can have on BG control. Insulin is the main hormone involved in glucose
regulation and homeostasis. It is released from the pancreatic beta cells in response to elevations
in BG, thereby helping glucose become properly stored in the liver in the form of glycogen,
which may be used when required. In addition, insulin allows the cells in the body to obtain
energy by assisting carbohydrates and fats in becoming absorbed and used effectively. Insulin
signals glucose-transport proteins to help distribute glucose throughout the body
efficiently. These glucose-transport proteins are dependent on adequate potassium to do their
job; so, if potassium is low, glucose metabolism may be affected. Increased body fat will also
interfere with insulin action, causing resistance to the action of the hormone, making it more
difficult to properly keep BG in balance. Glucagon is the opposing hormone to insulin and is also
produced in the pancrase, thereby inducing gluconeogenesis and other mechanisms to raise BG in
response to hypoglycemia.
It is not possible in the scope of this activity to cover every medication that may affect BG
metabolism. This activity, though, will highlight some of the more common medications
traditionally used in practice. Keep in mind that medications and/or factors that can alter BG metabolism and raise blood sugars may have the potential to affect patients with existing
diabetes and may also create conditions that lead to new-onset diabetes in certain at-risk
individuals.
Conditions That Affect Tests to Monitor Diabetes
The blood test for glycosylated hemoglobin (HbA1c) allows HCPs to have an indicator of
glycemic control over a period of approximately 3 months and has become the standard-of-care
measure for how well patients are controlling their diabetes. HbA1c is a stable glycoprotein
formed when glucose binds to hemoglobin in the blood. The average life span of a red blood cell
(RBC) is approximately 3 months, which is why HbA1c is a measure indicative of a 3-month
period.3 This test is also used to help confirm a diagnosis of diabetes, as well as assess a patient
with diabetes to determine therapy goals. The American Diabetes Association (ADA) has stated
that an A1C level of 7 or lower is a basic target for adult patients with diabetes. Some major
clinical trials, such as the Diabetes Control and Complications Trial (DCCT) and the United
Kingdom Prospective Diabetes Study (UKPDS) determined that good diabetes control, as
indicated by a lower HbA1c level, correlated with fewer complications in a patient with
diabetes.4 Therefore, it is crucial that the HbA1c level drawn and measured is accurate. If this
level is artificially higher or lower, it will inappropriately change therapy. The HbA1c level can
be affected by any process that lowers the life span of RBCs or makes a higher percentage of
young RBCs. Processes, such as acute blood loss or hemolysis, can dramatically alter the age
range of circulating RBCs, which will cause an inaccurate HbA1c reading.5
Iron deficiency anemia is seen in practice as the result of multiple factors, including small
bleeds, such as those caused by ulcers for example, and sometimes even dietary deficits. This
type of anemia can cause HbA1c levels to be falsely elevated.6 It is also important to note that
diabetes is a major cause of end-stage renal disease, with anemia being common in this patient
population because the kidneys control RBC production.
Hemolysis is a condition that reduces the RBC life span, which increases the proportion of
younger, less mature RBCs.6 If that life span is reduced, the resultant A1C value can be falsely
lowered. Drug-induced immune-mediated hemolysis is rare, but should not be overlooked.
Common drugs, which range from antibiotics like penicillin to Parkinson’s disease treatments
like methyldopa (Aldomet) and levodopa (Dopar), can cause this reaction. Even more common
medications—ibuprofen (Motrin), diclofenac (Cambia, Cataflam, Solaraze, Voltaren, Zorvolex),
and cephalosporins—have been implicated. Importantly, take a closer look at a patient profile if
an individual experiences a sudden unexpected change in his or her HbA1c level. If this occurs, a
practitioner has to be aware that hemolysis may be contributory, so further work-up should be
done.7-9 Drugs that are commonly associated with bleeding include nonsteroidal anti-inflammatory drugs (NSAIDs) and aspirin, meaning that patients on these medications who have
changes in their bowel habits and HbA1c levels also warrant further evaluation.10
Second-Generation Antipsychotics
Medications alter more than just how we measure glycemic control. Certain drugs have been
shown to dramatically affect glycemic control itself. A large population of patients with diabetes
experience depression or other forms of mental illness. Overall, people with T2DM have a 2-fold higher incidence of depression than the general population, with 1 study finding occurrences in 24% of women and 13% of men.11,12 Depression is a major comorbid condition, so we should
be aware of the potential side effects of agents commonly used to treat psychiatric illnesses.
The second-generation antipsychotic medications are notorious for negatively affecting blood
sugars and this class of agents has even been implicated as a cause of new-onset diabetes for
some patients. These drugs initially were touted as being better tolerated by patients because they
were associated with fewer extrapyramidal adverse events. The lower risk for these negative side
effects came with a cost, however. These medications are strongly associated with accelerated
weight gain, insulin resistance, diabetes, dyslipidemia, and increased cardiovascular risk. These
adverse effects can develop in as few as 6 months after the initiation of pharmacotherapy for
those without preexisting diabetes.13 Second-generation antipsychotic medications may cause
abnormal glucose metabolism that can lead to insulin resistance and T2DM; therefore, it is
imperative that patients with severe mental illness who are placed on chronic antipsychotic
medications, such as those listed in Table 1, be screened for diabetes.14 Pharmacists can assist
with identifying individuals who may be appropriate for screening, thereby helping with an early
diagnosis. A consensus statement has been developed by the ADA, in conjunction with other
professional organizations, which provides recommendations for monitoring fasting BG levels
for 12 weeks after starting therapy and annually, thereafter, for patients without preexisting
diabetes.15 If blood sugars move out of acceptable ranges, it may be prudent to switch a patient to
an antipsychotic, such as aripiprazole or ziprasidone, that is less likely to cause abnormalities in
blood sugars.
| Table 1 |
| First-Generation Antipsychotics |
Second-Generation Antipsychotics |
| Chlorpromazine (Largactil, Thorazine) |
Aripiprazole (Abilify) |
| Trifluoperazine (Stelazine) |
Olanzapine (Lanzek, Ozace, Zypadhera, Zyprexa) |
| Perphenazine (Trilafon) |
Quetiapine (Seroquel) |
| Haloperidol (Haldol) |
Paliperidone (Invega) |
| Thioridazine (Mellaril) |
Ziprasidone (Geodon, Zeldox) |
| Fluphenazine (Modecate, Prolixin) |
Risperidone (Risperdal, Zepidone) |
| |
Clozapine (Clozaril) |
For those patients who have already been diagnosed with diabetes and who are being prescribed
antipsychotic medications for the first time, it is important to discuss possible changes in diabetes
control with them. The second-generation antipsychotic medications, as stated, are of particular
concern. It is known that some antipsychotic agents cause weight gain, which, of course, affects
insulin resistance.16 The increase in weight caused by antipsychotic medications is often
unpredictable. Clozapine (Clozaril) and olanzapine (Lanzek, Ozace, Zypadhera, Zyprexa) cause
the greatest rise in weight, while aripiprazole (Abilify) leads to less of a gain.17 There seem to be other mechanisms, besides weight gain, that are involved in the development of diabetes in
patients using some antipsychotic medications, but these have not yet been fully
elucidated. Table 2 shows the extent to which some of these medications can cause an increase
in weight and possibly alter lipid metabolism as well.
Although the risk of developing diabetes is high for individuals on antipsychotic medications,
there is not enough screening of these patients. In late 2003, the U.S. Food and Drug
Administration (FDA) announced that it was requiring class warnings to be added to the labeling
of atypical or second-generation antipsychotic drugs, describing increased risks of
hyperglycemia and diabetes. In some cases, the hyperglycemia was profound and subsequently
associated with ketoacidosis, hyperosmolar coma, or death.18 The results of a recent time-series
analysis of over 100,000 Medicaid patients who are taking second-generation antipsychotic
medications showed that, despite the warning announced by the FDA, most individuals do not
typically receive baseline serum glucose and lipid testing.19 There has to be better screening, and
that starts with educating both HCPs and patients. Keep in mind that these drugs have helped
thousands of people to overcome severe mental illness, so careful attention to the benefit-versus-risk profile is a must for patients on these medications. There are no absolutes in medicine, so all
warnings and precautions have to be heeded.
| Table 2 |
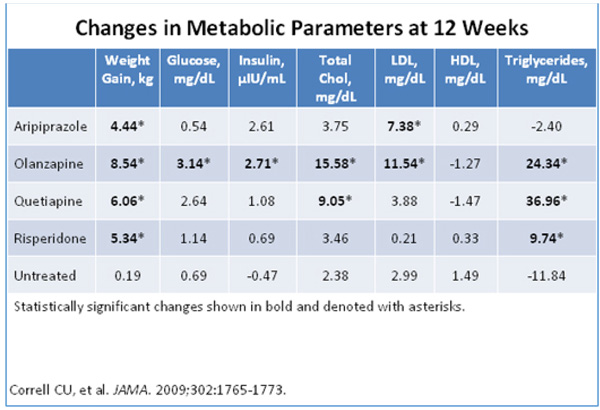 |
Chol = cholesterol; HDL = high-density lipoprotein; LDL= low-density lipoprotein
Correll CU, Manu P, Olshanskiy V, et al. Cardiometabolic risk of second-generation antipsychotic
medications during first-time use in children and adolescents. JAMA. 2009;302(16):1765-1773. |
Lipid-Lowering Agents
Another class of medications that has been shown to interfere with diabetes control is that of the
lipid-lowering drugs—specifically niacin (Niacor, Niaspan) or nicotinic acid, which has been
commonly used in the management of hyperlipidemia and focuses directly on
triglycerides. Diabetes and the metabolic syndrome are associated with elevated lipid profiles, so
many of your patients with diabetes may use some form of either prescription or over-the-counter niacin. In several studies, though, niacin has been reported to worsen diabetes control.20
One 16-week study that can be referenced concerning the effects of niacin at different doses on
BG control involved 148 patients with diabetes and evaluated such control as one of the
endpoints. The higher doses of niacin – 1000 to 1500 mg daily – resulted in an average HbA1c
increase of 0.3%. A recent meta-analysis of niacin users that looked at cardiac risk and diabetes
risk endpoints showed niacin therapy to be associated with a moderately increased risk of
developing the disease regardless of background statin.20 These results indicate we also have to
be more diligent at screening patients on niacin for new-onset diabetes, though no official
recommendations have been published yet.
Niacin is not the only lipid-lowering agent that interferes with glycemic control. Statins, which
are the most commonly prescribed medication for high cholesterol, have also been implicated in
altering glucose metabolism. In 2012, the FDA released changes in statin safety labels to include
those agents that have been found to increase HbA1c and fasting serum glucose levels.
Numerous studies that were done to ascertain a reduction in cardiac risk factors also found that
statins have diabetogenic potential and the effect varies with the dosage and type used.21 The
exact mechanisms have not yet been fully fleshed out, but some have proposed that statins
downregulate glucose transporters. Statins have also been shown to worsen diabetes control
in patients with preexisting disease, but these effects appear to be minimal, with solid evidence
not yet available.
Immunosuppressants: Corticosteroids and Transplant-Related Regimens
Perhaps the most notorious offending drug class of medications for altering glucose metabolism
in patients with diabetes and prediabetes are corticosteroids, which come in the form of oral and
inhaled medications as well as injectables in the hospital setting. Oral and intravenous
corticosteroids in some circumstances are unavoidable; they are excellent medications for
treating inflammatory or autoimmune conditions, such as chronic obstructive pulmonary disease
exacerbations, asthma, vasculitis, or even severe osteoarthritis. With that said, it is even more of
a necessity to understand the effect these drugs have on diabetes control and to counsel patients
accordingly.
The mechanisms for the influence of corticosteroids on glucose regulation are complex and
multifactorial. Glucocorticoids promote gluconeogenesis in liver and decrease glucose uptake
and utilization by antagonizing the insulin response in skeletal muscle and fat tissue.
Glucocorticoids also regulate glycogen metabolism in the liver by increasing glycogen storage.
In skeletal muscle, glucocorticoids permit the breakdown of glycogen, thereby resulting in higher
circulating levels of glucose. Even more importantly, glucocorticoids directly modulate the
function of pancreatic alpha and beta cells that normally regulate the secretion of glucagon and insulin.22 During a normal stress response, the body has to have excess glucose immediately. But
when this pathway is artificially stimulated, it can lead to cataclysmic effects on glycemic
control, commonly making glucose levels uncontrollable in a patient with diabetes within hours
of starting on an oral corticosteroid. It is incumbent on the pharmacist to advise patients with
diabetes that their blood sugar control will probably change, so a plan should be in place to
modify insulin dosing or medication, if necessary, after collaborating with their primary care
practitioner.
There have been myriad studies illustrating the correlation between hyperglycemia and
corticosteroid use. In 1 such study of patients with rheumatoid arthritis, nearly 9% developed
diabetes within the 2 years after starting glucocorticoid therapy, which was significantly higher
than the control group not on corticosteroid therapy.23 Another study showed that in patients
without diabetes but with primary renal disease treated with prednisolone, 42% were found to
have 2-hour post-lunch plasma glucose concentrations higher than 200 mg/dL, although they had
normal fasting glucose levels prior to starting the corticosteroid. In a case-controlled study, the
odds ratio of starting an oral hypoglycemic agent or insulin was 1.77 for those receiving a
hydrocortisone-equivalent dose of 1 to 39 mg/day, 3.02 for 40 to 79 mg/day, 5.82 for 80 to 119
mg/day, and 10.34 for 120 mg/day or more.24,25 For people who will require chronic immune
suppression with corticosteroids after transplantation, there are published guidelines on
managing glucocorticoid-related diabetes. Guidelines suggest checking the fasting plasma
glucose level once a week for the first 4 weeks after transplantation, then at 3 months, then at 6
months, and then once a year thereafter.26 Diabetes is the leading cause of end-stage renal
disease (ESRD) in the U.S., accounting for more than 44% of all patients with ESRD.
Transplantation is recommended, if possible, over dialysis because of improved morbidity and
mortality.27
It is also important to note that new-onset diabetes after transplantation, often referred to in the
literature as the acronym NODAT, is a serious complication. Once again it is evident that certain
medications have the ability to either potentially worsen diabetes control or actually cause new-onset diabetes in patients. It appears that immunosuppressant therapy in addition to oral
corticosteroids may act as triggers in developing diabetes in certain at-risk individuals, where
risk factors such as age, family history, and certain antibody titers are measured.28 Different
drugs were studied and compared for their ability to potentially contribute to new-onset diabetes
for patients who have had a transplant. Though all antirejection agents can have an effect on
BG metabolism, some may affect BG more than others. For example, cyclosporine was less
diabetogenic than tacrolimus. Transplant patients are on complex drug regimens and must be
monitored frequently for disease progression and signs of rejection.
Antihypertensive Medications
Approximately one-third of all adults in the U.S. have hypertension, and that number continues
to grow with our aging population. The number of adults with high blood pressure (BP) grew
from about 59 million to more than 70 million over the past decade. More important to this
discussion is that from 2009 to 2012, of those 18 years of age or older with diagnosed diabetes,
71% had BP higher than or equal to 140/90 mm Hg.29 With so many patients with diabetes being
treated for hypertension, it is quite common to see a prescription for a thiazide diuretic on a
patient profile.
Thiazide diuretics have been implicated in causing hyperglycemia in patients with diabetes and
also contributing to new-onset diabetes in some individuals. The exact mechanism of how
thiazide diuretics cause alterations in BG metabolism is poorly understood and the science
behind alterations in transporters is beyond the scope of this module. Some theories that have
been postulated include worsening of insulin resistance, decreasing insulin release, lowering
serum potassium, and activating the renin angiotensin-aldosterone system.30 Hydrochlorothiazide
has been implicated as a cause of new-onset diabetes in as few as 9 to 18 weeks after initiation of
therapy. Keeping patients on a lower dose of hydrochlorothiazide (12.5 to 25 mg) may help
ameliorate the chances of blood sugar issues in patients with or without preexisting diabetes.
HCPs may also opt to choose a different class of medication or a potassium-sparing diuretic if
diabetes and hyperglycemia are concerns.31,32
Beta-blockers are another class of antihypertensive agents that, like thiazide diuretics, have been
found to raise the risk of developing diabetes and possibly affect blood sugar control in patients
with diabetes. As pharmacists, we have always been taught that beta-blockers can mask the signs
of hypoglycemia by slowing the heart rate and blunting sympathetic response to low blood sugar.
The main mechanism for increasing insulin resistance is vasoconstriction of small blood vessels
in muscle tissue, which impairs glucose transport across the vascular membrane.33 New-onset
diabetes is also increased in those on beta-blockers by more than 30% for yet-to-be-clarified
reasons. While beta-blockers have a profoundly positive effect on reducing cardiac morbidity
and mortality, we cannot forget the consequences of these medications on glycemic control and
act accordingly.34
HIV Medications
Protease inhibitors (PIs) are a mainstay of HIV therapy and this category of medications has
been shown to cause hyperglycemia in patients with and without diabetes. PIs acutely and
reversibly inhibit the insulin-responsive glucose transporter Glut 4, in turn leading to peripheral
insulin resistance and impaired glucose tolerance.35 Animal models have also shown direct
pancreatic beta-cell dysfunction.36
Antibiotics
Those with diabetes are more prone to infections than those without the disease. Persistent
hyperglycemia creates an environment ripe for bacteria to grow and a suppressed immune
system in these patients significantly heightens the risk of serious infection for those with
diabetes over the general population.37 Therefore, antibiotics are often a staple of therapy for
most people with diabetes at some time in their lives. Thus, it is crucial to realize that certain
antibiotics may cause serious BG fluctuations in this group of patients.
There is also an elevated risk of BG fluctuations in patients with diabetes who take
fluoroquinolones, as shown by a study that involved over 78,000 people with diabetes in
Taiwan. The study looked at these patients’ use of the following 3 classes of antibiotics:
fluoroquinolones, macrolides, and cephalosporins. An endpoint was any emergency-department
list or hospitalization for severe blood sugar swings within 1 month (30 days) after starting the
antibiotics.38 The study’s results showed that those patients on fluoroquinolones were more likely
to experience severe blood sugar swings than those who took other classes of antibiotics. The
odds of severe hypoglycemia and hyperglycemia were significantly greater with (levofloxacin
(Levaquin), but not ciprofloxacin (Cipro, Cipro XR, Proquin XR), than with azithromycin (Zithromax, Zmax). Moxifloxacin (Avelox, Vigamox) was implicated as causing the highest risk
for hypoglycemia.39
To learn how the fluoroquinolone class causes these metabolic derangements, the studies
referenced above point toward the important role of the adenosine triphosphate (ATP)-sensitive
K+ channels in the pancreatic beta cell and the importance of anti-insulin hormones. In any
event, this study shows that caution should be exercised when patients with diabetes are started
on any fluoroquinolone.
In addition, a recent study done at the University of Texas linked metronidazole (Flagyl,
Metrogel, Noritate), fluconazole (Diflucan), and sulfamethoxazole-trimethoprim (Zotrim) to
episodes of hypoglycemia in patients with diabetes who were taking oral antihyperglycemic
agents, such as glipizide (Glucotrol, Glucotrol XR) and glyburide (DiaBeta, Micronase). In
conclusion, more frequent monitoring of blood sugars is recommended if a patient taking a
sulfonylurea is also prescribed an antibiotic associated with hypoglycemia.40
Diabetes is a complex disease that requires a great deal of thought when evaluating blood sugars.
If a patient with diabetes has an illness, his or her blood sugar will likely rise in response to the
stress on the body. Once an antibiotic is given, it is possible that blood sugars will normalize
because the patient is “getting better.” The above antibiotics may be useful for treating patients
with diabetes and are certainly not contraindicated, but caution is advised in making sure blood
sugar fluctuations are not extreme.
Other Common Drugs: Alcohol and Caffeine
The most commonly abused psychotropic drugs in the U.S. are actually caffeine and alcohol.
The U.S. Department of Health and Human Services recommends a maximum of 1 drink per day
for women and 2 drinks daily for men. A single drink is defined as 12 ounces of beer, 5 ounces
of wine, or 1.5 ounces of spirits. Excess alcohol consumption is dangerous enough for the
general population, but adding diabetes to the equation makes the situation even more
treacherous.41
While drinks do carry carbohydrate value, which can contribute to overall blood sugar control,
one of the biggest issues with drinking and diabetes is the potential for hypoglycemia, where
blood sugar drops too low. This risk can carry over for 8 to 10 hours after you drink alcohol. For
most people, this risk for hypoglycemia happens at night, when the patient is most vulnerable.
Alcohol becomes metabolized in the body in a manner that makes it especially dangerous for a
patient with diabetes. When alcohol is ingested, most of the metabolic capacity of the liver is
involved, so even if hypoglycemia is treated with complex carbohydrates, the effect may not
manifest for hours. Also, glucagon will not work as effectively after alcohol consumption,
thereby leading to an impaired sympathetic response to low blood sugar. To add to the
confusion, alcohol’s neurologic effects may be confused with signs of hypoglycemia.42
Caffeine is certainly a staple of many people’s morning ritual. Consumption of this stimulant is
known to raise blood pressure (BP), but caffeine has also been shown to potentially raise BG. Paradoxically, caffeine has also been lauded as possibly helping to prevent T2DM. There is
really not enough evidence to show clear results either way because studies did not take into
account other factors, such as how long a person has been consuming coffee or what types of coffee are consumed. A small study that was published in Diabetes Care in 2007 looked at the
effects of black coffee on blood sugar levels. Higher glucose levels were found in those study
participants given caffeine versus those given placebo.43 A proposed mechanism of caffeine
thought to cause a rise blood sugars may involve the stimulant causing the release of
epinephrine, which can increase BG through hormonal regulation. Interestingly enough, caffeine
was theorized to help prevent the development of T2DM. Results at this point are inconclusive,
so we should continue to preach moderation with this commonly used agent.
Conclusions
Patients with diabetes often have other comorbidities that must be treated as well. This often
leads to polypharmacy, which has been defined as 1 patient on 5 or more clinically relevant
prescription medications. Our senior population is growing, currently comprising some 14% of
the U.S. population and making up approximately 34% of prescription-drug users.
With the expanding role of the pharmacist in the new health care landscape, it is incumbent on
the pharmacist to identify potential adverse drug reactions (ADRs) and to report them when
necessary. ADRs are the 4th leading cause of hospital admissions, which is significant because
many of the ADRs are preventable. With medication therapy management (MTM) at the
forefront of pharmacy practice, pharmacists can make a huge impact on the nation’s
health. Regular documentation and identifying potential drug therapy issues will surely become
the new business model.
The complexity of drug regimens in the patient with diabetes creates an increasing challenge for
the pharmacist who is completing a Comprehensive Medication Review and identifying the
person’s risks and benefits of medication therapy. Also, because of the increasing older adult
population, medications that are appropriate for a given senior patient may be incorrectly dosed
for that patient. In a study conducted at a Veterans Affairs Medical Center in Michigan, patients
with diabetes were found to have experienced potentially dangerous hypoglycemia because their
medications were potentially dosed too high.44
Senior citizens often require lower dosing of agents because they typically have lower body mass
indexes and, therefore, metabolize drugs differently than younger patients. Lower dosing of
medications in this ever-growing older patient population is often warranted.
As we have seen throughout this module, medications that cause alterations in BG are often
implicated in new-onset diabetes, especially in those patients at high risk for developing the
disease. It is important to know the symptoms of diabetes, which include polydipsia, polyuria,
polyphagia, and sudden weight loss or frequent urinary tract infections. Armed with the proper
information, we can all make interventions to potentially save lives.
| Counseling Tips for Common Drugs that Affect Diabetes Control |
| Category |
Potential Counseling Tips |
| Testing |
- The blood test for glycosylated hemoglobin (HbA1c or A1C) is a measure of glycemic control over 3 months.
- An A1C level of 7 or lower is a basic target for adult patients with diabetes.4
|
| Conditions that can alter A1C readings |
- The HbA1c level can be affected by any process that lowers the life span of red blood cells (RBC) or makes a higher percentage of young RBCs. These conditions include Iron deficiency anemia among others.6
|
| Medications that impact glycemic control |
- Certain drugs have been shown to impact glycemic control.
- Medications that can negatively impact blood sugars include: second-generation antipsychotic medications can negatively impact blood sugars, niacin, statins, transplant medications, certain blood pressure medications (e.g., thiazides and Beta-blockers), certain medications for HIV (human immunodeficiency virus), caffeine and alcohol.
|
Update on Niacin Use
In 2016, the Food and Drug Administration (FDA) withdrew approval of the indications related to the coadministration of niacin extended-release (ER) tablets with a statin.1 This decision was based on results from two large clinical event trials, Atherothrombosis Intervention in Metabolic Syndrome With Low HDL/High Triglycerides: Impact on Global Health Outcomes (AIM-HIGH) and Heart Protection Study 2–Treatment of HDL to Reduce the Incidence of Vascular Events (HPS2-THRIVE), which concluded that niacin added to statin therapy did not provide clinical event benefit over statin alone.2 The ADA states that “Combination therapy (statin/niacin) has not been shown to provide additional cardiovascular benefit above statin therapy alone, may increase the risk of stroke with additional side effects, and is generally not recommended”.3
References:
1. https://www.federalregister.gov/documents/2016/04/18/2016-08887/abbvie-inc-et-al-withdrawal-of-approval-of-indications-related-to-the-coadministration-with-statins;
2. Superko HR, Zhao XQ, Hodis HN, Guyton JR. Niacin and heart disease prevention: Engraving its tombstone is a mistake. J Clin Lipidol. 2017;11(6):1309-1317;
3. American Diabetes Association. 9. Cardiovascular disease and risk management: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018;41(Suppl. 1):S86–S104.
|
REFERENCES
- Dennis Thompson: Prescription Drug Use Continues to Climb in U.S. HealthDay Reporter WEDNESDAY, May 14, 2014. http://consumer.healthday.com/senior-citizen-information-31/misc-aging-news-10/prescription-drug-use-continues-to-climb-in-u-s-687822.html. Accessed Feb 2016.
- Nolan L, O’Malley K. Prescribing for the elderly. Part 1: Sensitivity of the elderly to
adverse drug reactions. J Am Geriatr Soc. 1988;36(2):142-149.
- Bry L, Chen PC, Sacks DB. Effects of hemoglobin variants and chemically modified
derivatives on assays for glycohemoglobin. Clin Chem. 2001;47(2):153-163.
- The Diabetes Control and Complications Trial Research Group. The effect of
intensive treatment of diabetes on the development and progression of long-term
complications in insulin-dependent diabetes mellitus. N Engl J Med.
1993;329(14):977-986.
- Goldstein DE, Little RR, Lorenz RA, et al. Tests of glycemia in diabetes. Diabetes
Care. 1995;18(6):896-909.
- Tarim O, Küçükerdoğan A, Günay U, et al. Effects of iron deficiency anemia on
hemoglobin A1c in type 1 diabetes mellitus. Pediatr Int. 1999;41(4):357-362.
- Arndt PA, Garratty G. The changing spectrum of drug-induced immune hemolytic
anemia. Semin Hematol. 2005;42(3):137-144.
- Garratty G, Arndt PA. An update on drug-induced immune hemolytic anemia. Immunohematology. 2007;23(3):105-119.
- Garratty G. Immune hemolytic anemia associated with drug therapy. Blood Rev.
2010;24(4-5):143-150.
- Bjarnason I, Hayllar J, MacPherson AJ, Russell AS. Side effects of nonsteroidal anti-inflammatory drugs on the small and large intestine in humans. Gastroenterology.
1993;104(6):1832-1847.
- Ali S, Stone MA, Peters JL, et al. The prevalence of co-morbid depression in adults
with type 2 diabetes: a systematic review and meta-analysis. Diabet Med. 2006;23(11):1165-1173.
- Baumeister H, Hutter N, Bengel J. Psychological and pharmacological interventions
for depression in patients with diabetes mellitus and depression. Cochrane Database Syst Rev. 2012;12:CD008381.
- Rojo LE, Gaspar PA, Silva H, et al. Metabolic syndrome and obesity among users of
second generation antipsychotics: a global challenge for modern
psychopharmacology. Pharmacol Res. 2015;101:74-85.
- Ramaswamy K, Masand PS, Nasrallah HA. Do certain atypical antipsychotics
increase the risk of diabetes? A critical review of 17 pharmacoepidemiologic studies. Ann Clin Psychiatry. 2006;18(3):183-194.
- Hasnain M, Fredrickson SK, Vieweg WV, Pandurangi AK. Metabolic syndrome
associated with schizophrenia and atypical antipsychotics. Curr Diab Rep. 2010;10(3):209-216.
- Jesus C, Jesus I, Agius M. What evidence is there to show which antipsychotics are
more diabetogenic than others? Psychiatr Danub. 2015;27 Suppl 1:S423-S428.
- Correll CU, Manu P, Olshanskiy V, et al. Cardiometabolic risk of second-generation
antipsychotic medications during first-time use in children and adolescents. JAMA.
2009;302(16):1765-1773.
- Bushe CJ, Leonard BE. Blood glucose and schizophrenia: a systematic review of
prospective randomized clinical trials. J Clin Psychiatry. 2007;68(11):1682-1690.
- Morrato EH, Druss B, Hartung DM, et al. Metabolic testing rates in 3 state Medicaid
programs after FDA warnings and ADA/APA recommendations for second-generation antipsychotic drugs. Arch Gen Psychiatry.2010;67(1):17-24.
- Goldie A, Taylor AJ, Nguyen P, et al.. Niacin therapy and the risk of new-onset
diabetes: a meta-analysis of randomised controlled trials. Heart. 2016;102(3):198-203.
- Chogtu B, Magazine R, Bairy KL. Statin use and risk of diabetes mellitus.” World J
Diabetes.2015);6(2):352-357.
- Kuo T, McQueen A, Chen TC, Wang JC. Regulation of glucose homeostasis by
glucocorticoids. Adv Exp Med Biol. 2015;872:99-126.
- Panthakalam S, Bhatnagar D, Klimiuk P. The prevalence and management of
hyperglycaemia in patients with rheumatoid arthritis on corticosteroid therapy. Scott
Med J. 2004; 49(4):139-141.
- Uzu T, Harada T, Sakaguchi M, et al. Glucocorticoid-induced diabetes mellitus:
prevalence and risk factors in primary renal diseases. Nephron Clin Pract. 2007;
105(2):c54-c57.
- Gurwitz JH, Bohn RL, Glynn RJ, et al. Glucocorticoids and the risk for initiation of
hypoglycemic therapy. Arch Intern Med. 1994;154(1):97-101.
- Davidson J, Wilkinson A, Dantal J, et al; International Expert Panel. New-onset
diabetes after transplantation: 2003 International consensus guidelines. Proceedings of
an international expert panel meeting. Barcelona, Spain, 19 February 2003.
Transplantation. 2003;75(10 Suppl):SS3-SS24.
- Stewart JH, McCredie MR, Williams SM, et al. Trends in incidence of treated end-stage renal disease, overall and by primary renal disease, in persons aged 20-64 years
in Europe, Canada and the Asia-Pacific region, 1998-2002. Nephrology (Carlton). 2007;12(5):520-527.
- Chan CM, Chim TM, Leung KC, et al. Simultaneous pancreas and kidney
transplantation as the standard surgical treatment for diabetes mellitus patients with
end-stage renal disease. Hong Kong Med J. 2016;22(1):62-69.
- Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United
States: National Health and Nutrition Examination Survey, 2011-2012. NCHS Data
Brief, No. 133. Hyattsville, MD: National Center for Health Statistics, Centers for
Disease Control and Prevention, US Dept of Health and Human Services; 2013.
- Palmer BF. Metabolic complications associated with use of diuretics. Semin Nephrol.
2011;31(6):542-552.
- Bell DS. Treatment of diabetic hypertension. Diabetes Obes Metab. 2009;11(5):433-444.
- Taylor EN, Hu FB, Curhan GC. Antihypertensive medications and the risk of incident
type 2 diabetes. Diabetes Care. 2006;29(5):1065-1070.
- Fonseca V, Bakris GL, Bell DS, et al. Differential effect of beta-blocker therapy on
insulin resistance as a function of insulin sensitizer use: results from GEMINI. Diabet Med. 2007;24(7):759-763.
- Jacob S, Rett K, Henriksen EJ. Antihypertensive therapy and insulin sensitivity: do
we have to redefine the role of beta-blocking agents? Am J Hypertens.
1998;11(10):1258-1265.
- Carr A, Samaras K, Burton S, et al. A syndrome of peripheral lipodystrophy,
hyperlipidaemia and insulin resistance in patients receiving HIV protease inhibitors. AIDS. 1998;12(7):F51-F58.
- Murata H, Hruz PW, Mueckler M: The mechanism of insulin resistance caused by
HIV protease inhibitor therapy. J Biol Chem. 2000;275(2):20251-20254.
- Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: a
review of pathogenesis. Indian J Endocrinol Metab. 2012;16 Suppl 1:S27-S36.
- Aspinall SL, Good CB, Jiang R, et al. Severe dysglycemia with the fluoroquinolones:
a class effect? Clin Infect Dis. 2009;49(3):402-408.
- Coblio NA, Mowrey K, McCright P, et al. Use of a data warehouse to examine the
effect of fluoroquinolones on glucose metabolism. Am J Health Syst Pharm. 2004;61(23):2545-2548.
- Parekh TM, Raji M, Lin Y, et al. Hypoglycemia after antimicrobial drug prescription
for older patients using sulfonylureas. JAMA Intern Med. 2014;174(10):1605-1612.
- Crocq MA. Alcohol, nicotine, caffeine, and mental disorders.” Dialogues Clin
Neurosci. 2003;5(2):175-185.
- Richardson T, Weiss M, Thomas P, Kerr D. Day after the night before: influence of
evening alcohol on risk of hypoglycemia in patients with type 1 diabetes. Diabetes Care. 2005;28(7):1801-1802.
- Whitehead N, White H. Systematic review of randomised controlled trials of the
effects of caffeine or caffeine drinks on blood glucose concentrations and insulin
sensitivity in people with diabetes mellitus. J Hum Nutr Diet. 2013;26(2):111-125.
- Sussman JB, Kerr EA, Saini SD, et al. Rates of deintensification of blood pressure
and glycemic medication treatment based on levels of control and life expectancy in
older patients with diabetes mellitus. JAMA Intern Med. 2015;175(12):1-8.
Back to Top