
Expired activity
Please go to the PowerPak
homepage and select a course.
Module 5, Part 1. Communication Essentials: Tips for Patient and Care Giver Communication
How Communication in MTM Differs from Basic Pharmacist Counseling Services
Pharmacists are trained in patient counseling and communicating health information to the public. Medication therapy management (MTM) offers a chance to provide patient counseling at a higher level, with greater opportunity for give-and-take dialogue. Interactions with the patient during MTM go beyond the product-oriented counseling pharmacists provide on a daily basis.
When engaging in counseling with patients, pharmacists often want to pass along their own ideas or suggestions to the patient. In MTM, the idea is to find out what the patient's goals are, and to look for ways to address that individual's unique needs and problems. The process is more of an interactive collaboration between the patient and the pharmacist, rather than simply delivering information. To start, the pharmacist should think in terms of two basic questions for the patient:
- If there is one issue we can address related to your medicines, what would it be?
- What is the most important thing you want to get out of our visit today?
Table 1 illustrates the different stages of patient-pharmacist communication, from basic transfer of information (first column) to a more interactive level of communication with MTM counseling (column on far right).
| Table 1. Stages of Patient-Pharmacist Communication |
| |
Information Transfer |
Information Exchange |
Patient
Education |
MTM |
| Level of information |
Brief, non-individualized |
Detailed, individualized |
Comprehensive: may be group or individualized |
Detailed information exploration and guidance |
| Spontaneous or planned |
Spontaneous, i.e., related to filling a prescription |
Spontaneous or planned |
Planned |
Planned |
| Goal/objective |
Basic information needed to use medication as directed (monologue) |
Pharmacist responds to and asks questions about medication
(dialogue) |
Collaborative learning environment (conversation) |
Guidance that assists in fulfilling needs for managing a medical condition (discussion) |
| Benefit to patient |
Safe, proper use of a medication or product |
Patient receives more individualized information about use of medication |
Increases condition-specific knowledge about proper use of medications |
Enhances problem-solving skills and assists with management of condition |
| Nature of relationship |
Passive instruction |
Active exchange of information |
Interactive learning |
Interactive collaboration and discussion |
Adapted from: United States Pharmacopeia (USP) Medication Counseling Behavior Guidelines.
USP DI update, Vols. I and II. Rockville, MD: United States Pharmacopeial Convention; 1997:
664-675 |
Product counseling vs. MTM
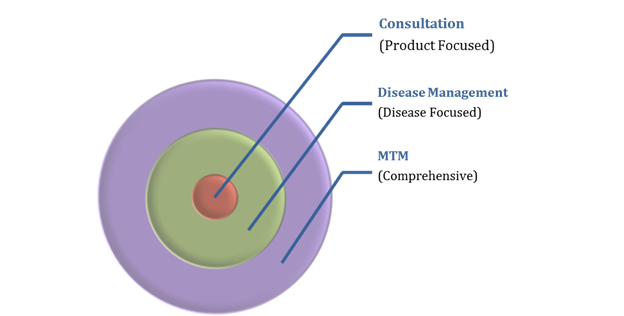
At the pharmacy counter, patients frequently answer "No" when asked if they have any questions about new or renewed medications. People often answer "no" because they don't recognize how the added insight about their medication could help them to manage their medical condition. This is a classic case of "We don't know what we don't know." Your patient may not be looking at the big picture, which is that he or she has not considered whether or how well their medications are working for them. The average patient probably does not know enough about medicines to ask the right kinds of questions, and thus relies on the pharmacist or other health professional to inform them.1 However, the patient may sense that the doctor does not have time to answer all of their questions, and may assume this is true of the pharmacist as well. Most of these counseling opportunities are product-specific and targeted to the specific issues with one medication. Generally they do not include a comprehensive evaluation of the whole patient and the entire medication regimen (Figure 1).
Figure 1. Medication Therapy Management (MTM) Vs. Other Forms of Pharmacist Counseling
Patients who are unclear about the benefits of single-product counseling are also likely to be uncertain about a comprehensive MTM visit. However, when questions about a medication are put into the context of a person's own lifestyle, the rationale for MTM becomes clearer. "Do you forget to take this medication? What complications do your medications cause? Do you have side effects that cause you to use it in a different way than as directed? Do you have concerns about the possible long-term effects of this medicine? Are high copayments or lack of coverage preventing you from filling the prescription? Do you cut pills in half, cut back on doses, or otherwise alter the prescription to fit your schedule, lifestyle, or budget?" These are the types of issues that MTM can help bring to light.
Introducing the goals and benefits of MTM
To begin an MTM session, it may be helpful to very briefly explain to the patient the purpose of the MTM process and why it is worth their time and attention. Table 2 contains "Frequently Asked Questions" that can be used or adapted to share with patients about the goals, benefits, and steps of MTM.
| Table 2. Frequently Asked Questions About Medication Therapy Management (MTM) |
|
What is MTM?
Medication therapy management (MTM) is a service provided by a healthcare professional (often a pharmacist) to help patients gain the best possible benefits from their medications. This is usually done during a meeting between the pharmacist and the patient or a caregiver. A main goal of MTM is to identify, prevent, and resolve medication-related problems.
Why do I need MTM?
Almost anyone who receives medical therapy for a chronic illness or medical condition can benefit from MTM services. Usually, MTM is offered for people who have multiple medical conditions or are taking several medications. MTM is also helpful after a person has been hospitalized or has a change in medical care providers. People who are having problems with taking their medicines correctly are often helped by MTM services. Even if you don't know whether you need MTM, you may be surprised at what you can learn from the process.
What should I expect during an MTM counseling session?
It is always best to have a face-to-face meeting with the MTM provider. If that is not possible, a phone or videoconference may be substituted. The pharmacist or other MTM provider will tell you what you need to bring to the meeting. At a minimum, you should bring all of your medications with you to the first visit (over the counter and prescription). During the meeting, you will have a chance to sit down with the pharmacist to discuss your questions and problems. You may talk about your health, your medicines, and ongoing needs. This may be different from what you have done with your doctor, because it is more focused on medications and how to use them correctly.
Is MTM a one-time meeting, or a longer-term process?
In order to be effective, MTM services need to involve a follow-up plan. How often you will meet with the pharmacist or exchange information will vary for each individual. A main goal of MTM is to produce changes that can benefit the person over a long-term period.
How does my doctor find out about changes in medical care determined during an MTM session?
The pharmacist providing the MTM services will follow up with your physician and/or other healthcare providers. There are certain changes that the doctor may need to authorize. Also, it is important that the doctor's records match with yours and those of the pharmacist. It can sometimes be helpful if you let your doctor know that you have participated in an MTM consultation and request his or her cooperation with the process.
|
For patients who are unfamiliar with MTM, the pharmacist can briefly explain that MTM is:
- Proven effective in helping patients better manage their health
- Different from other pharmacist counseling
- Designed to focus on the individual's chief concerns and questions
- Designed to streamline and simplify the individual's treatment, not to complicate or make more work for the patient
- Improve outcomes of drug therapy
How to Improve Communication Skills for Patient Counseling
Communicating clearly with patients has been part of the educational curriculum for pharmacists for decades, but studies of real life pharmacist–patient encounters suggest that many pharmacy professionals need to improve communication skills.2,3 In the text Communication Skills in Pharmacy Practice, Beardsley and colleagues note, "Many pharmacists have not practiced these skills to the point they are comfortable applying them."4 The result is that pharmacists "either avoid uncomfortable situations or they hesitate or 'freeze' when confronted with a new situation." According to these authors, changing communication behaviors involves:
- Awareness (knowing what should be done differently)
- Practicing new skills (using the new strategy)
- Assessing the approach (determine what went well and what needs to be improved)4
Role-playing scenarios (such as those taught to improvisational actors) can help pharmacists to spot communication mistakes and identify why certain statements might be confusing or off-putting to the patient. The scenario shown below was used in a 4-year study from Finland on patient communication.1
- Pharmacist: Here is your medicine. Are you familiar with this product?
- Patient: No, I'm not.
- Pharmacist: Did your doctor talk to you about how to use the medicine?
- Patient: I think so.
- Pharmacist: Should I open the package and show you?
- Patient: I don't know.
- Pharmacist: Well, please be sure to read the leaflet in the package.
According to the report, this scenario might occur in any country and illustrates a "robotic approach" that highlights many gaps in communication competency:
- The patient is giving clear hints of the need for education, but the pharmacist is unaware of the need (asks closed-ended questions), or unable to follow through on this need.
- The pharmacist asks questions, but does not know how to make use of the patient's answers.
- The patient indicates this is a new medication, but the pharmacist does not provide instruction on how to use it.
- The pharmacist creates a confusing situation by leaving the decision up to the patient about whether a demonstration should be given.
- The pharmacist makes the assumption that the patient:
- 1) will read the package insert;
- 2) can read and understand English; and
- 3) can understand and apply the information about the drug.
- Pharmacists may use jargon, acronyms, or terms the patient does not understand. The educational material included with the prescription is long and is often intimidating or confusing to the patient.
Assessments of pharmacist communication practices have shown that the most effective interactions tend to occur when the pharmacist is demonstrating a certain skill (such as how to use an inhaler device) or answering specific questions (such as what side effects a medication might cause). Initiating an open-ended conversation about the patient's needs and customizing the message to fit the individual are areas where the most improvements may be needed.1 Communication and interviewing skills for pharmacists often mirror those taught to physicians and other healthcare professionals. The American Association of Medical Colleges (AAMC) provides the mnemonic, SEGUE, to summarize core competencies in patient communication (Table 3).5
| Table 3. Core Competencies in Patient Communication |
|
The "SEGUE" framework for teaching and assessing communication skills
Set the Stage
- Greet the patient appropriately
- Establish the reason for visit
- Outline the agenda for visit
- Make a personal connection
- Maintain privacy
Elicit Information
- Elicit the patient's view of health problems and/or progress
- Explore physical/physiological factors
- Explore psychosocial/emotional factors
- Discuss previous treatments
- Discuss how health problems affect the patient's life
- Discuss lifestyle issues/prevention strategies/health risks
- Avoid directive/leading questions
- Give the patient opportunity/time to talk
- Listen. Give the patient undivided attention
- Check/clarify information
Give Information
- Explain rationale for diagnostic procedures
- Teach the patient about his/her own body and situation
- Encourage the patient to ask questions
- Adapt to the patient's level of understanding
Understand the Patient's Perspective
- Acknowledge the patient's accomplishments/progress/challenges
- Acknowledge waiting time
- Express caring, concern, empathy
- Maintain a respectful tone
End the Encounter
- Ask if there is anything else the patient would like to discuss
- Review next steps with the patient
|
| Source: American Association of Medical Colleges (AAMC). Communication in Medicine.5 |
The pharmacist can use steps in the Segue Framework to collect information, but to gain further understanding about how to help patients change their habits and behaviors, the concept of motivational interviewing is involved.
Motivational Interviewing Techniques
Motivational interviewing is a counseling method that helps address people's unwillingness or inability to change something about themselves. In MTM, this technique can be used to help patients improve medication adherence and overcome resistance to a new or difficult medication or healthcare procedure. More information about motivational interviewing can be found in the Adherence module of this certificate program.
The key principles of motivational interviewing are:6,7
- Develop a relationship with the person
- Express empathy (offer acceptance and understanding)
- Develop a discrepancy (that is, help patients to see the difference between what they want and what they are doing)
- Roll with resistance (confront the problem, not the person; understand that resistance is likely to occur and often stems from fear of change)
- Support self-efficacy (promote belief in the person's ability to change; identify previous successful experiences.
In MTM, the patient interview should begin with open-ended questions ("Tell me how you take this," not "So, you're taking this twice a day?") and progress to closed-ended questions in order to clarify or fine-tune certain points. The pharmacist should be open to letting the patient talk openly—addressing the patient's chief concerns first—while steering the person back on track if needed. Some concepts of "motivational interviewing" initially developed by Miller and Rollnick are applicable to MTM.8 These are:
- Ask open-ended questions
- "How does this medicine make you feel?" NOT: "Do you feel nauseated when you take
the medicine?"
"What would you like to get out of this session today?" NOT: "I think you might be able
to benefit from...."
- Reflect back what the person has said:
- "It sounds like the stress you're experiencing is making it harder for you to manage your
pain." NOT: "You can't let the stress stop you from taking care of yourself."
- Periodically sum up what has been said:
- "So, in the morning you might skip a dose because you feel the medicine upsets your
stomach."
Active listening techniques
Active listening refers to the ability of a listener to not only hear another person's words, but to understand the complete message being sent.9-11 Much of the listening we do is actually spent tuning out the speaker, making our own inferences about the message, and jumping ahead to plan our own responses. The principles of active listening can be taught—and practiced—in order to improve communication in the context of MTM. The 5 key elements of active listening are outlined in Table 4.
| Table 4. 5 Key Elements of Active Listening9-11 |
| 1. Focus on giving the speaker your undivided attention |
DO:
- Acknowledge the message.
- Look directly at the speaker
- Put aside distracting thoughts
|
DON'T:
- Mentally prepare a response
- Tune in to outside distractions such as other conversations
|
| 2. Give cues to show that you are listening |
DO:
- Use both nonverbal (body language) and verbal cues
- Nod occasionally, smile, use other facial expressions to convey attention
- Adjust posture to convey an inviting, open message
|
DON'T:
- Use "negative" facial cues, such as eye-rolling or yawning
- Fidget (e.g., play with a desk accessory)
|
| 3. Provide verbal and nonverbal feedback |
DO:
- Give the speaker occasional indicators that you understand what is being said.
- Reflect back, paraphrasing what the speaker has said. Use phrases such as "What I'm hearing is..." or "It sounds like you are saying..."
- Ask questions to clarify the speaker's intent. "What do you mean when you say...? or "Is this what you mean?" Ask for examples: "Can you give me an example of what you mean when you say you feel 'lousy'?")
|
DON'T:
- Interrupt the speaker
- Go off on a tangent when the goal is to validate what the person is saying
|
| 4. Avoid being judgmental |
DO:
- Keep in mind that the speaker's point of view may not reflect your own.
- Allow a person to vent frustrations about the healthcare system or a chronic disease
|
DON'T:
- Present counterarguments when the speaker is telling his or her point of view
- Cast blame. Instead of "I can't believe he did that," you could say, "That must have been frustrating for you."
|
| 5. Respond appropriately |
DO:
- Be candid, open, and honest
- Assert opinions and advice thoughtfully. Try "I would like to suggest that..." rather than "This is what you should be doing."
|
DON'T:
- Over-state what you have heard
|
Barriers and Pitfalls in Patient Communication
"The single biggest problem in communication is the illusion that it has taken place." —George Bernard Shaw
Few MTM sessions go "by the book." It is more likely that the pharmacist will encounter a number of communication challenges or barriers with each patient encounter. These challenges may include:
- Visual, hearing, or cognitive impairment
- Low literacy (poor or no reading skills) and/or low health literacy
- Language barriers (low English proficiency)
- Different cultural beliefs about health and disease
More detailed discussion on overcoming barriers, including literacy and health literacy issues is provided in the upcoming module (Module 14) on Adherence.
Telephone Encounters
Telephone encounters are a cornerstone of MTM interventions. As many as 92% of MTM encounters occur over the telephone, while 40% of plans also provide the opportunity for face-to-face visits.12 Additionally, follow-up arrangements after a face-to-face MTM encounter usually occur via phone. Pharmacists should recognize several important considerations in a successful telephone encounter. These include:
- Prepare for the telephone encounter by gathering information you wish to discuss with the patient
- Ensure a quiet environment and ensure you have time to speak to the person on the phone
- Avoid speakerphones when possible, to ensure patient privacy and good sound quality
- Introduce yourself and the purpose of the call
- Use a clear and pleasant voice (try smiling when speaking) and enunciate words clearly
- Use active listening and reflective questioning (i.e., "Yes, I understand," "Tell me more about that," or "I understand you are having trouble affording your medications. How can I help you with that?"
- Avoid slang and abbreviations; communicate in a health literate manner
- Try not to interrupt or cut the person off while he/she is speaking
- If you need to place the person on hold, explain what you are doing, why, and how long they can expect to wait for you. (Try not to leave a person on hold for longer than 15–20 seconds without offering to call them back)
- Ask for clarification if you are not sure what the person is saying
- Summarize your discussion and determine next steps for you and for the patient
- Employ the teach back method to ensure the patient understands what was discussed
- Determine if a follow-up phone call is necessary and establish a time and date to follow-up
- Document your telephone encounter and share it with the patient's other providers
Summary and Conclusions
Education about how to communicate better with patients is a part of the pharmacist's training but should be an ongoing process. As this module highlights, the need for sensitive, empathetic, and effective communication with patients and caregivers is heightened during the process of MTM, because there is a much greater need for give-and-take of information. Communication skills such as using open-ended questions and active listening are an important part of MTM, but the pharmacist also needs to hone the skills of keeping the communication exchange focused and goal-oriented.
References
- Wuliji T, Airaksinen M. Counselling, Concordance, and Communication: Innovative Education for Pharmacists. International Pharmaceutical Federation. 2005.
- Boesen KP, Herrier RN, Apgar DA, et al. Improvisational exercises to improve pharmacy students' professional communication skills. Am J Pharm Educ. 2009;73(2):35.
- Kimberlin CL. Communicating with patients: skills assessment in US colleges of pharmacy. Am J Pharm Educ. 2006;70(3):67.
- Beardsley RS, Kimberlin CL, Tindall, WN. Communication Skills in Pharmacy Practice. 6th ed. Philadelphia: Wolters Kluwer Health; 2011.
- Association of American Medical Colleges. Report III. Contemporary Issues in Medicine: Communication in Medicine. 1999. Washington, D.C. .
- Miller NH. Motivational interviewing as a prelude to coaching in healthcare settings. J Cardiovasc Nurs. 2010;25(3):247-251.
- Levensky ER, Forcehimes A, O'Donohue WT, et al. Motivational interviewing: an evidence-based approach to counseling helps patients follow treatment recommendations. Am J Nurs. 2007;107(10):50-58; quiz 58-59.
- Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol. 2009;64(6):527-537.
- Davidhizar R. Listening--a nursing strategy to transcend culture. J Pract Nurs. 2004;54(2):22-24; quiz 26-27.
- Robertson K. Active listening: more than just paying attention. Aust Fam Physician. 2005;34(12):1053-1055.
- Fassaert T, van Dulmen S, Schellevis F, et al. Active listening in medical consultations: development of the Active Listening Observation Scale (ALOS-global). Patient Educ Couns. 2007;68(3):258-264.
- Centers for Medicare & Medicaid Services. 2013 Medicare Part D Medication Therapy Management (MTM) Programs. Fact Sheet: Summary of 2013 MTM Programs. Sept 12, 2013..
Back to Top