
Expired activity
Please go to the PowerPak
homepage and select a course.
Dehydration: New Approaches to an Age-Old Problem
INTRODUCTION
Day in and day out, from birth to death, the human body tightly regulates water balance through natural processes that take place largely without deliberate thought or intervention. Still, dehydration—a decrease in total body water that affects physiologic function—is a common condition that contributes to morbidity and mortality in millions of people worldwide each year. Dehydration may be the result of disease, water deprivation, drugs, exertion, or microbes.
With the pharmacy the most accessible health care setting, pharmacists and pharmacy technicians are well positioned to recognize patients with and at risk for dehydration. Pharmacists can recommend products for most mild cases and many moderate cases of dehydration and can refer patients with more severe cases for medical or emergent care. This type of pharmaceutical care can only be provided if pharmacists and technicians have adequate information about water, glucose, and electrolyte homeostasis; a knowledge of contemporary ideas about interventions for dehydration; and access to currently recommended products for preventing and treating dehydration.
This article provides information for pharmacists and pharmacy technicians regarding potential signs and symptoms of dehydration in various types of patients, possible etiologies of dehydration, and patients at high risk for the condition. Pathophysiologic consequences of dehydration and related fluid and electrolyte imbalances will also be presented, along with the role of oral replacement therapy (ORT) solutions for preventing and treating dehydration. The module will also discuss the development of care plans for patients with or at high risk for dehydration, including individuals using select over-the-counter (OTC) products and those who should be referred for medical care.
EPIDEMIOLOGY AND ETIOLOGY OF DEHYDRATION
Water is an essential nutrient and is the only liquid that is necessary for life. The human body regulates the amount of water it contains through homeostatic responses to changes in plasma osmolality; it can compensate for a decline of as little as 1% in body water (e.g., 700 grams in a 70-kg person) within 24 hours.1 Depending on the reason for the water loss, electrolytes may have been lost or become concentrated, which can lead to relative deficiencies and excesses. Hypovolemia refers to the loss of water and electrolytes; dehydration is a decrease in total body water with or without changes in electrolytes.
Dehydration is diagnosed when total body water decreases by 3% or more. The factors listed in Table 1 are used to determine the severity of the water loss. Dehydration severity is associated with a greater degree of skin, cardiovascular, and fluid status signs and symptoms.1-5
| Table 1. Signs and symptoms of dehydration according to severity of water loss1-5 |
| Signs and symptoms |
Mild dehydration |
Moderate dehydration |
Severe dehydration (medical emergency) |
| Decrease in body weight |
3% – 5% |
6% – 10% |
11% – 15% |
| Thirst |
Dry, sticky mouth; feeling thirsty |
Dry, sticky mouth; feeling thirsty |
Very dry mouth, skin, and mucous membranes; extreme thirst |
| Affect |
Dizziness, lightheadedness, sleepiness, tiredness |
Dizziness, lightheadedness, sleepiness, tiredness |
Delirium or unconsciousness |
| Face/head |
Normal |
Sunken eyes |
Sunken eyes; in infants, sunken fontanels |
| Skin |
Normal |
Decreased turgor and prolonged capillary refill time; pale color |
Markedly decreased turgor and prolonged or minimal capillary refill time; mottled or gray color; parched appearance |
| Hemodynamic changes |
Normal pulse and blood pressure |
Slightly increased pulse |
Tachycardia; low blood pressure and possible cardiovascular collapse |
| Respiration |
Normal |
Normal to fast |
Hypercapnia; deep breathing |
| Urine and body fluid status |
Mild oliguria; decreased tears |
Oliguria |
Anuria; no tears |
Dehydration can be associated with many contributory factors, including water deprivation, excessive sweating from heat and/or exercise, vomiting or diarrhea, fever, or excessive urination from diseases such as diabetes or the use of drugs such as diuretics, caffeine, alcohol, or antibiotics that cause diarrhea. Chronically low fluid intake is associated with conditions such as urolithiasis, constipation, asthma, cardiovascular disease, diabetic hyperglycemia, and some cancers.6
Symptoms of dehydration include dry or sticky mouth, rapid heart rate, low blood pressure, lack of tears, low or no urine output for 8 hours with dark yellow color of urine, sunken eyes, and dizziness.2 Water deprivation can lead to death in a matter of days, and outcomes of dehydration can be particularly serious or severe in vulnerable patients such as infants (i.e., from birth to 1 year of age), young children, older patients (i.e., those who are 65 years of age or older), and individuals with poor health.6
Worldwide, diarrhea in children younger than 5 years is a major cause of morbidity and mortality. Infants and children are particularly susceptible to gastrointestinal pathogens, which can lead to acute gastroenteritis and diarrhea, and they can quickly develop dehydration from these causes.5 Infants are more susceptible to dehydration and its consequences than adults because water comprises a higher percentage of infant body weight (i.e., 75%) and infant kidney function is less developed than in adults. Additionally, the metabolic rate of infants is higher than that of adults, infants cannot express thirst or obtain fluids on their own, infant formula may be insufficiently diluted, and infants are more susceptible to fluid loss secondary to fever, vomiting, and diarrhea than adults.1,4,7
ORT, which is discussed in more detail later in this module, has greatly reduced morbidity and mortality among young children from diarrhea-producing diseases such as cholera and rotavirus infections. In the past 2 decades, worldwide deaths from all causes in children younger than 5 years old decreased from 12 million in 1990 to 6.9 million in 2011 as rotavirus and pneumococcal vaccines became more widely used and more effective distribution systems for ORT were developed.8,9
In the United States (U.S.), a common cause of dehydration among people of all ages is traveler’s diarrhea, which is most often caused by enterotoxigenic Escherichia coli.4,7,10 (E. coli is the causative pathogen in up to 72% of cases of traveler’s diarrhea.) Traveler’s diarrhea is treated with fluid replacement, as well as antibiotics to treat the E. coli infection.11 Compared with other patient groups, infants are at highest risk of developing traveler’s diarrhea.4,7,10 Diarrhea caused by antibiotic-associated changes in intestinal flora is also a common cause of dehydration in infants and young children.12
Pregnant women are prone to morning sickness and vomiting, which can cause dehydration. An obstetrician–gynecologist or other medical professional should manage these conditions, particularly when emesis is severe enough to cause dehydration.
Older patients are also at risk of experiencing dehydration. In this patient population, the thirst sensation declines, the kidneys produce less concentrated urine and are more resistant to the effects of antidiuretic hormone (vasopressin; ADH), and renin activity and aldosterone secretion decline. Age-related physiologic factors and comorbidities are also factors that contribute to dehydration: decreased mobility, changes in vision, swallowing disorders, cognitive decline, and sedative use all contribute to older adults’ impaired abilities to sense the need for fluids and/or to obtain them.1
Caffeine, alcohol, and medications such as diuretics can also produce dehydration. During international travel by air, dehydration can develop from a combination of factors: low humidity of cabin air that increases respiratory water loss, inadequate water intake, increased intake of diuresis-producing caffeine and alcohol, and altered sleep/wake cycles that affect dietary and fluid consumption.13
Excessive alcohol intake can also cause dehydration. Despite its ubiquity, the alcohol “hangover” is poorly understood. Research into its exact cause has yielded conflicting results, with some studies pointing to a relationship between dehydration and the symptoms of a hangover. Whether dehydration is the cause of a hangover, or a condition that occurs simultaneously with the hangover, lay people and medical professionals alike generally believe that increased water and fluid intake before, during, and after alcohol consumption decreases the occurrence and severity of hangover symptoms.14-16
PATHOPHYSIOLOGIC CONSEQUENCES OF DEHYDRATION
The body regulates and maintains plasma osmolality between 280 to 295 mOsm/kg. At approximately 285 mOsm/kg, sensations of thirst develop and the secretion of ADH signals the kidney to reduce urine output. The small intestine plays a major role in sodium homeostasis by reabsorbing secreted sodium using a glucose-enhanced, sodium-potassium-activated ATPase pump located in the intestinal lining. Impairment of this pump is the mechanism by which cholera produces its profuse, rice water diarrhea.17
Three different types of dehydration, each caused by a different mechanism, can affect the body’s physiology.18 Treatments differ according to type, so recognizing the cause of dehydration is important. As noted earlier, dehydration is a decrease in water content of the body. When electrolyte loss accompanies water loss, the condition is referred to as isotonic dehydration or hypovolemia. Water in the body is either extracellular or intracellular; isotonic dehydration is a decrease in extracellular fluid (ECF) volume. Profuse diarrhea can cause this type of dehydration.1 Hypertonic dehydration results from inadequate water intake or excessive water loss. Vomiting and sweating cause a loss of fluids that are hypotonic, which produces hypertonic dehydration. Other causes of hypertonic dehydration include water deprivation, impaired consciousness, osmotic diuresis, or diuresis from conditions such as diabetes insipidus (including medication-induced diabetes insipidus).1,18
During extended or extreme exertion, or during exercise in hot and humid conditions, replacement of sweat loss with large amounts of pure water can lead to hypotonic dehydration. The excessive amount of water consumed—similar to situations of water intoxication—can cause the osmolality of the ECF to drop, causing a shift of water to the intracellular spaces to maintain osmotic balance. This situation is more likely to occur in elite athletes than in the general population, including most children and adolescents participating in recreational sports, but hypotonic dehydration is a medical emergency when it occurs. Hypotonic dehydration can also develop after replacement of hypotonic or isotonic gastrointestinal fluid loss with large amounts of pure water.1,19
Patient reports of symptoms that are suggestive of dehydration (Table 1) are difficult to interpret since many of the symptoms are nonspecific. The most important indicator of acute dehydration is a decrease in body weight following vomiting, diarrhea, exertion, or other contributing situation. For example, athletes who report a weight loss of 2 kg during a 2-hour afternoon workout have likely lost approximately 2000 mL of water, and this weight loss is a reliable indicator of the need for replacement therapy.
Despite the nonspecific nature of most symptoms of mild and moderate dehydration, their impact should not be minimized. Cognitive performance declines with mild or moderate dehydration in young children and older adults, but also in otherwise healthy young adults.20 Frail older people are susceptible to adverse effects of acute dehydration, with increased mortality reported during abnormally warm weather and increased risks of acute medical conditions during periods of acute dehydration.6
ORT SOLUTIONS
Until the efficacy of ORT was recognized in the 1960s, cholera was a death sentence for many patients, especially in medically underserved areas where the infection was endemic. Up to half of patients with severe cases of the disease died from profound dehydration within 12 hours of its onset. Medical researchers had previously identified effective ways to bypass the gastrointestinal tract with intravenous (IV) fluids and electrolytes to replenish water and sodium in patients with cholera, but these approaches were thwarted by nonsterile preparations and unbalanced compositions during cholera outbreaks in developing countries. Initial attempts at administering oral electrolyte solutions failed because of immediate reflexive vomiting.21
The full story of the development of ORT and its recognition as one of the 20th century’s most important medical advances22 is beyond the scope of this article, but pharmacists and pharmacy technicians should understand the basic principles of how ORT works in patients with cholera and the ways in which those principles were applied to the treatment of diarrhea in infants. This experience and knowledge provides some of the best evidence for how dehydration occurs, the impact it has on the body, and the best methods for treatment.
Development and importance of ORT solutions
To develop effective ORT solutions, researchers first had to overcome many misconceptions about cholera. In the 1800s, for example, the disease was thought to destroy the gastrointestinal tract, but, by the 1960s, IV replacement therapy was refined as a treatment for cholera that reduced mortality to nearly zero. However, replacement volumes of up to 40 L of sterile fluids depleted available supplies in areas where cholera was common. The challenge was to convert replacement therapy to something that could be used in settings with limited medical resources.21
Oral administration of an electrolyte solution was tested in patients whose reflexive vomiting was controlled by initial IV therapy, but investigators found that the body did not absorb sodium and potassium after oral administration. One simple ingredient—glucose—was missing, they later found. A retired U.S. Navy Captain, Robert A. Philips, MD, reported that patients who consumed a balanced glucose–electrolyte solution experienced less diarrhea, more rapid rehydration, and faster recovery than patients receiving traditional electrolyte solutions and other forms of fluid replacement.23 Glucose is a transporter that facilitates electrolyte and water absorption from the gastrointestinal tract, so glucose-containing ORT solutions were able to compensate for the cholera toxin–induced fluid loss and prevent dehydration while the Vibrio cholerae organism was eliminated from the body.21
The simple but profound medical advance of ORT was thus born. Bags of salts could be prepared, distributed, and stored in cholera-endemic areas, ready for dissolution in clean water at the first hint of a cholera outbreak. In 1969, the World Health Organization (WHO) designated oral rehydration salts (ORS) as a nonproprietary name for a balanced glucose–electrolyte mixture that was approved, recommended, and distributed by United Nations Children’s Emergency Fund and WHO.24 In 2003, WHO changed the composition of ORS solutions on the basis of research showing that the original formula was not optimal and, in 2006, WHO provided further guidance on the use of ORS (Table 2).24 The new formulation has a reduced osmolarity and contains less sodium and glucose than the original product. Compared with the original formulation, the new formulation is associated with reduced vomiting, decreased stool output, lower risk of hypernatremia, and less frequent need for IV infusions. ORS solutions are used worldwide to treat cholera, other types of diarrhea, and dehydration from other causes.25
| Table 2. Composition of oral replacement solutions19,22 |
| Component |
New formula (adopted in 2003 and modified in 2006) |
Previous formula |
| Sodium chloride (g/L) |
2.6 |
3.5 |
| Glucose, anhydrous (g/L) |
13.5 |
20 |
| Potassium chloride (g/L) |
1.5 |
1.5 |
| Trisodium citrate, dihydrate (g/L) |
2.9 |
2.9a |
| Total osmolarity (mOsm/L) |
245 |
311 |
| aCould be replaced by the same amount of sodium bicarbonate. |
Clinical use of glucose and electrolyte therapy
The clinical scenarios associated with ORT are limited to fluid and electrolyte loss from diarrhea or vomiting (generally isotonic hypovolemia, with the possibility of accompanying metabolic acidosis or alkalosis), but several parallels exist between cholera and the various physiologic factors involved in other types of dehydration. Experiences with cholera treatment are useful in determining how to treat dehydration caused by other factors.
For oral treatment of isotonic hypovolemia, replacement of water and electrolytes must be facilitated by the administration of glucose. Another consideration is that in patients with hypertonic dehydration from vomiting, sweating, or water deprivation, water replacement is often sufficient treatment. Unless the sweating resulted from extensive exertion or exercise, oral therapy for glucose and electrolyte replenishment is not needed; electrolytes are not depleted, and normal meals with accompanying healthy drinks are generally sufficient to replace expended energy sources. Finally, hypotonic dehydration is generally a medical emergency and may require initial therapy with hypertonic fluids followed by isotonic products.
ASSESSMENT OF FLUID AND ELECTROLYTE STATUS IN CHILDREN AND ADULTS
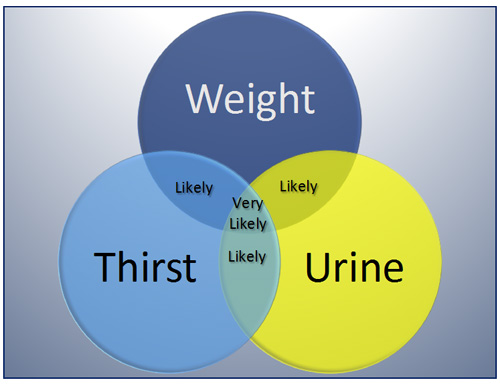
Pharmacists may or may not have access to patients’ serum electrolyte measurements, but pharmacists in ambulatory care settings (e.g., community pharmacies and ambulatory clinics) can combine several assessment techniques to determine the hydration status of adults and children who present with signs and symptoms suggestive of dehydration (Table 1) and a clinical history of fever, exertion, vomiting, diarrhea, or diuresis. As outlined below for different patient groups, 3 key indicators of hydration status are weight, urine output and color, and thirst. Figure 1 illustrates the likelihood of dehydration on the basis of objective changes in weight and urine output combined with subjective feelings of thirst.26,27 Changes in a single variable are not a reliable indicator of dehydration. If 2 indicators are present, dehydration is likely, and, if all 3 are present, a patient is very likely dehydrated.26 If other symptoms and assessment factors listed in Table 1 are also present without an alternative clinical explanation, the pharmacist can proceed with a working diagnosis of dehydration and make reasonable recommendations for self-care therapies or transfer to an emergency department.
| Figure 1. "WUT" mnemonic to assess the likelihood of dehydration on the basis of acutely reduced body weight, changes in urine output and color, and the presence and nature of thirst sensation26,27 |
 |
Assessing hydration status in infants, children, and adolescents
For infants and young children presenting in ambulatory pharmacy settings with symptoms of acute gastritis or other conditions associated with changes in water and electrolyte basis, total body weight is an especially important indicator of dehydration. These patients lack awareness of and ability to express the sensation of thirst, which limits the utility of that indicator, and the use of diapers compromises assessment of urine volume and color. Parents and other caregivers can be questioned about the usual and recent numbers of wet diapers per day; a substantial decline could mean that dehydration is developing. If a measurement of urine output is available, less than 1 mL/kg/h indicates oliguria in infants; for older children, oliguria is a urine output of less than 0.5 mL/kg/h. Light, straw-colored urine indicates that the patient is well hydrated; the darker the urine, the more likely that dehydration is present.28,29
Physical examination of pediatric patients of all ages can also provide clues to hydration status. In addition to changes in respiratory or heart rates, increases in the time required for skin to recoil after pinching (reflecting skin elasticity or turgor) is associated with dehydration. "Tenting” of the skin of the abdominal wall at the level of the umbilicus also indicates dehydration. Capillary refill time (i.e., the time required for color to return to the skin after pressure is exerted to produce blanching of the skin on the sternum of infants and fingernail beds, fingers, or arms of older children) can also be used to measure hydration status: a refill time of more than 1.5 to 2 seconds frequently occurs with dehydration.28,29 Dehydration of 5% or more is likely if more than one of these indicators is positive for dehydration. Patients with this level of dehydration may be progressing quickly toward severe dehydration, which indicates a need for medical or emergent attention.29
Assessing hydration status in adults
When combined with clinical history, the triad of weight, urine, and thirst can be used to assess hydration status of adults of all ages. Young and middle-aged adults with stable weights can rely on acute changes in weight during a period of vomiting, diarrhea, or exertion as an indicator of a potential water deficit. Adults with less than 400 to 500 mL urine output per 24 hours are considered to have oliguria, which indicates moderate dehydration. Anuria (i.e., the production of extremely low volumes of urine—less than 50 mL/d in an adult) indicates severe dehydration. As with pediatric patients, light, straw-colored urine indicates that the patient is well hydrated; the darker the urine, the more likely that dehydration is present.
Thirst while at rest is a strong indicator of dehydration in young and middle-aged adults. However, thirst is not usually perceived until a loss of 2% of total body water has occurred, limiting its usefulness. Additionally, the thirst sensation subsides before the body is fully rehydrated.26 Similar to pediatric patients, skin recoil time in adults is increased with dehydration.
Patients with unexplained symptoms of dehydration may require medical evaluation for renal and endocrine causes of the condition. The pharmacist should review the patient’s medication list for diuretics or other medications that could alter water and electrolyte homeostasis. The pharmacist can also ask about lifestyle factors that could cause dehydration, such as the consumption of large amounts of caffeine or alcohol or poor water intake.
The hydration status of older adults, especially those with dementia, can be difficult to evaluate. A recent Cochrane review showed that no individual test or combination of tests is reliable for identifying impending or current water-loss dehydration in older people. The authors concluded that “[the tests] miss a high proportion of people with dehydration and wrongly label those who are adequately hydrated.”30 Objective tests of serum electrolytes, renal function, and endocrine imbalances, in addition to complete medical histories, may be needed to evaluate hydration status in older patients.5
Assessing hydration status in athletes
For recreational and elite athletes who need to monitor hydration status during periods of intense or extended exertion, measuring body weight after voiding each morning provides a useful baseline estimate of total body weight and, therefore, total body water. If an individual’s post-exertion weight is more than 2% to 3% below the first morning body weight without any other explanation, dehydration is likely developing, especially when urine and thirst symptoms are also present. Spot measures of urine color or urine specific gravity have also been used for detecting dehydration, but these assessments have limitations and are not widely applied in assessments of hydration status.26
PREVENTION AND TREATMENT OF DEHYDRATION
Preventing dehydration is far preferable to treating it. The gap between adequate hydration and severe dehydration is narrow with a fluid-losing disease or activity. The example of cholera is illustrative of this point: patients can go from initial symptoms of dehydration to death in as few as 12 hours. To paraphrase the old saying, an ounce of prevention is worth a gallon of cure.
When making specific product or referral recommendations to patients, pharmacists should remember the goal of fluid replacement: restore and maintain physiologically appropriate levels of water and electrolytes in ECFs and interstitial spaces using the least invasive means to achieve optimal patient outcomes.
Self-care hydration products
Many choices for fluid replacement are available in both pharmacies and general retail outlets for consumers to use when dehydration is anticipated or present. These include water, balanced ORT products, and sports drinks. Consumers may incorrectly believe that energy drinks, teas, and colas are useful in this situation (Table 3).17,31-35
| Table 3. Contents of select rehydration solutions, sports drinks, and other drinks18,28,31-35 |
| Product |
Carbohydrate content
(g/L) |
Sodium
(mEq/L) |
Potassium
(mEq/L) |
Chloride/base
(mEq/L) |
Osmolarity
(mOsm/L) |
| Rehydration solutions (manufacturer) |
| CeraLyte 70 (Cera Products, Inc.) |
40 (rice starch polymers) |
70 |
20 |
30 |
220 – 235 |
| Enfamil Enfalyte (Mead Johnson Nutrition) |
N.D. (corn syrup solids) |
47 |
24 |
74 |
167 |
| Hydralyte (Hydralyte LLC) |
16 (dextrose) |
45 |
20 |
45 chloride; 90 citrate |
245 |
| Pedialyte (Abbott Global) |
25 (dextrose) |
45 |
20 |
35 |
270 |
| Sports and other drinks |
| Typical sports drink |
255 (variety of carbohydrate sources) |
20 |
3 |
2 |
360 |
| Powerade (The Coca-Cola Company) |
21 per serving (high fructose corn syrup) |
150 mg per serving |
35 mg per serving |
N.D. |
N.D. |
| Colas, regular |
High fructose corn syrup, sucrose |
2 |
0 |
13 |
550 – 700 |
| Tea |
None |
0 – 10 |
0 |
0 |
18 |
| Water |
None |
0 – 10 |
0 |
0 |
0 – 18 |
| Abbreviations: N.D., no data. |
Water. Patients can use water in many situations for preventing and treating dehydration. People of all ages who engage in recreational sports of less than 1 hour in duration and of low or medium intensity should use water to replenish fluid loss; electrolyte replenishment products are needed only if symptoms of dehydration are present or anticipated (on the basis of past experience).
The use of water to replace large volumes of fluid loss can lead to hypotonic dehydration or water intoxication. This can occur with fever, vomiting, diarrhea, or diuresis, or in older patients who rapidly replace fluids lost after acute or chronic periods of insufficient water intake. As explained in the next section, patients using water to replenish a deficit should ingest water over a 48-hour period with a normal diet (for electrolyte normalization).18
The choice between tap and bottled water is largely patient preference in the U.S., where most tap water is clean and safe. Bottled water is portable and may be more convenient, but it can present a substantial expense. Bottled water is necessary for residents of and visitors to areas without safe drinking water.
Balanced ORT products. For most disease- and medication-induced dehydration states, balanced ORT products are the mainstay of prevention and treatment of dehydration. As with the ORS formulations developed by WHO for the treatment of cholera, balanced ORT products are designed for safe and effective replacement of body fluids lost through vomiting, diarrhea, fever, water deprivation (including travel-related situations), excessive sweating, and diuresis.
ORT products marketed in the U.S. differ in osmolarity, carbohydrate content and source, and electrolyte composition (Table 3). Many, but not all, products are slightly hypotonic and, therefore, ideal for preventive or replacement therapy of mild or moderate isotonic and hypertonic dehydration.31-33
Dextrose is the most commonly used carbohydrate in commercial ORT products. It is preferred over sucrose, as the latter requires conversion to glucose for physiologic effect (i.e., enhanced absorption of sodium and potassium) and produces an osmotic diuresis if it reaches the colon unchanged. One product uses rice starch polymers, and another contains corn syrup solids; no head-to-head comparisons provide evidence of superiority of these carbohydrate sources and osmotically active ingredients. Electrolyte composition varies slightly, but not significantly, among available products.5,31-33
Some ORT products are available only as oral solutions, while others are also available as effervescent tablets, powders, and/or freezer pops. Various flavors are also available to facilitate administration, especially to infants and young children already irritable from fever, vomiting, or diarrhea.
ORT products should be administered according to age-specific dosing guidelines. Charts are available from several ORT manufacturers to log the amount and time of product administration, as well as urine output and episodes of vomiting, diarrhea, and fever.
Sports drinks. Sports drinks (i.e., beverages used for water and electrolyte replenishment during exercise) contain various combinations of carbohydrates, minerals, electrolytes, and flavoring. The American Academy of Pediatrics (AAP) recommends against the use of sports drinks in children and adolescents engaging in low or moderate intensity exercise, including recreational sports.19 As shown in Table 3, sports drinks contain large amounts of carbohydrates28,34,35; used in excess, these products can lead to an unrecognized and unnecessary increase in caloric intake.
The AAP Committee on Nutrition and the Council on Sports Medicine and Fitness issued a policy statement regarding sports drinks: “Sports drinks have an important, specific role in the diet of young athletes who are engaged in prolonged vigorous sports activity—primarily to rehydrate and replenish carbohydrate, electrolytes, and water lost during exercise. However, daily carbohydrate intake must be balanced with adequate intake of protein, fat, and other nutrients. In general, there is little need for carbohydrate-containing beverages other than the recommended daily intake of fruit juice and low-fat milk.”19 Sports drinks are also not appropriate for routine use by children and adolescents. In addition to excessive caloric intake, AAP warns that sports drinks are associated with dental erosion and enamel demineralization because of their low pH.19
Sports drinks should be used only in hydration management for elite athletes and those exercising or working in hot, humid environments for prolonged periods. Dehydration is known to impair athletic and cognitive performance,26 but the role of sodium supplementation for maintenance of hydration is controversial.36,37 The use of sports drinks in activities where large amounts of sweat are lost is reasonable but not supported by evidence. Sports drinks should not be used in most other situations where dehydration is likely or present, including vomiting, diarrhea, fever, or diuresis from medications or diseases.
Energy drinks. Energy drinks and sports drinks are very different product categories. The AAP policy statement explains that young people are not clear on the distinction between energy drinks and sports drinks.19 Unlike sports drinks, energy drinks contain various nonnutritive ingredients such as caffeine and other stimulants, guarana, taurine, ginseng, L-carnitine, creatine, and/or glucuronolactone. These ingredients are not appropriate for performance enhancement during exercise by children and adolescents, according to the AAP policy statement. Consumption of energy drinks has been associated with neurologic and cardiovascular adverse effects and can lead to physical dependence and addiction.19 Concerns similar to those expressed by AAP are pertinent for adults. Energy drinks have no place in maintaining or replenishing water and electrolytes lost through exercise, disease, medications, or any other cause.
Teas and colas. As shown in Table 3, the composition of teas and colas makes them inappropriate in hydration therapy. The carbohydrate content of many cola products is not appropriate in a healthy diet, the caffeine content is excessive given the amount of cola needed for treating dehydration, and the hypertonic composition of many colas actually worsens isotonic and hypertonic dehydration. Teas lack electrolytes (Table 3) but contain methylxanthine derivatives with stimulatory and diuretic properties that could worsen patients’ cognitiveand hydration status.35 Herbal teas can be used in small amounts as part of culturally appropriate or alternative medicine treatments.
Developing clinical plans for dehydration
Individualized hydration plans for patients must balance the many causes of water and electrolyte loss, patient age and conditions, and the possibility of other causes that might reflect systemic disease or organ dysfunction.
Clinical plans for infants, children, and adolescents. Pediatricians should generally manage water and electrolyte loss in infants, which is most frequently the result of acute gastroenteritis caused by viral or bacterial pathogens, fevers associated with otitis media or other infections, or diarrhea caused by antibiotics given for such infections. Self-care is not appropriate in most of these cases. Children older than 1 year and adolescents with mild or moderate dehydration can often be managed with self-care products, as long as parents and caregivers are aware of the need for medical attention if the cause of dehydration (e.g., vomiting or diarrhea) does not subside and/or progressive symptoms indicate the condition is worsening.
Infants aged 3 months or younger with diarrhea and fever of at least 38° C (100.4° F), emesis, lethargy, irritability, refusal to feed, or signs of dehydration should be referred for immediate pediatric care. Pediatricians will often manage older infants (up to 12 months of age) who have vomiting and diarrhea with ORT products until symptoms remit. Breastfeeding is typically continue as tolerated; formula-fed babies are often switched to ORT products until the normal diet can be resumed.38 Early refeeding can reduce the duration of symptoms by about a half day.5
Administration of ORT products to ill, fussy infants and young children can be difficult. Caregivers should frequently offer sips of these products with the goal of having the patient drink approximately 1 mL/kg of the product every 5 minutes. Several ORT manufacturers offer products as frozen pops; these can be used effectively in children.
Pediatric patients with acute gastroenteritis should be rehydrated rapidly; the Centers for Disease Control and Prevention recommends administration of replacement fluids over a 3- to 4-hour period. The Holliday–Segar method can be used to determine an adequate maintenance volume of fluid in children: the hourly water requirement for ORT products plus other fluids is 4 mL/kg for those weighing 10 kg or less (≤ 23 pounds), 40 mL plus 2 mL per kg for each kg between 11 and 20 kg for those weighing 11 to 20 kg (24 to 44 pounds), and 60 mL plus 1 mL/kg for each kg over 20 kg for those weighing more than 20 kg (44 pounds).28 If vomiting or diarrheal episodes continue, an additional 60 to 120 mL of ORT solution can be given for each episode for patients weighing less than 10 kg, and 120 to 240 mL of ORT solution per episode can be added for children weighing more than 10 kg.5
Older children and adolescents with fever, vomiting, or diarrhea should receive a balanced ORT product for prevention and treatment of mild or moderate dehydration.5 These products can also be used to prevent or treat dehydration associated with international travel or clinical conditions that produce losses of hypotonic body fluids through the skin, lungs, or gastrointestinal tract. As discussed above, children and adolescents should not use sports drinks unless they are engaged in prolonged (more than 1 hour) or intensive exercise or exertion, or are active in a very hot, humid environment.19
AAP does not recommend the use of antidiarrheal agents in pediatric patients; the drugs can produce serious adverse effects in infants and young children.5 Other than in cases of traveler’s diarrhea, antibiotics are not useful in pediatric patients with diarrhea, as they may worsen the symptoms by altering intestinal flora. In children who are placed on antibiotics (for other conditions), prophylactic probiotics can prevent or decrease severity of diarrhea.39
Exclusions to self-care in pediatric patients at risk for and with dehydration include age younger than 1 year, severe emesis that may produce metabolic alkalosis, severe diarrhea that could produce metabolic acidosis, and patients with signs or symptoms of severe dehydration (Table 1). As symptoms dictate, parents and caregivers should take pediatric patients for immediate pediatric or emergent care.19,38
Clinical plans for adults. Water is a suitable option for rehydration for adults of all ages in the vast majority of situations. Adults need only water with a normal diet, unless water and electrolyte losses are extreme because of exertion, exercise, disease, medication, or water deprivation.
In the ambulatory or community pharmacy setting, a balanced ORT product for prevention and treatment of mild or moderate dehydration can be recommended for patients with fever, vomiting, or diarrhea that is expected to create a substantial fluid deficit. Likewise, these products can be useful for adults during international travel or when alcohol, caffeine, or diuretic use creates symptoms of dehydration. As noted previously, these clinical conditions produce losses of hypotonic body fluids through the skin, lungs, and the gastrointestinal tract. Because of acid loss, severe emesis can produce metabolic alkalosis; severe diarrhea can lead to metabolic acidosis through loss of fluids with a high pH. If a patient’s pulse or respiratory rate is altered, indicating a metabolic condition, or if symptoms of severe dehydration are present (Table 1), the patient should be referred for medical or emergent care.
A minimum daily water intake of 1,500 to 1,600 mL is reasonable for most adult patients. Patients with water loss should consume a sufficient amount of water or ORT product beyond that normal daily requirement to replace the decrease in total body weight; for those with dehydration, 2 to 4 L of fluid is commonly needed. The replacement fluids should be ingested over a 4-hour period for acute losses. For each diarrheal or vomiting episode in adults, an additional 120 to 240 mL of replacement fluid should be consumed.
Patients with water deprivation, including older people whose intake has been chronically low, should ingest a replacement amount of water products over a 48-hour period while eating a normal diet. This will ensure adequate electrolyte replacement and avoid hypotonic hyponatremia. Alternatively, pharmacists can recommend a balanced ORT product if consumption of a normal diet is not feasible or assured or if faster replenishment is medically necessary or desired.
Patients with symptoms of dehydration not associated with an obvious cause may require medical evaluation for renal and endocrine causes. The pharmacist should review the patient’s medications for diuretics or other medications that could alter water and electrolyte homeostasis. The pharmacist can also ask about lifestyle factors that can cause dehydration, including consumption of large amounts of caffeine or alcohol or poor water intake. The pharmacist can make appropriate recommendations regarding daily water intake, consumption of a normal diet, and medications and suggest seeking medical care if symptoms worsen or do not subside.
To prevent and treat dehydration associated with diarrhea, the use of antidiarrheal agents, particularly the peripherally acting opiate loperamide, is an accepted part of treatment for nonspecific and traveler’s diarrhea in adult patients. It is dosed at 4 mg initially followed by 2 mg after each loose stool, with a maximum of 8 mg in a 24-hour period.40,41
Exclusions to self-care in adults with dehydration include those with severe or rapidly progressing symptoms and pregnancy. While balanced ORT products are safe to use in patients with mild or moderate dehydration (Table 1), those with severe dehydration should be referred for medical or emergent care. In addition, emesis in pregnant women should be monitored by the obstetric care provider. People with potentially systemic disease or medication use contributing to dehydration may require referral to a medical professional.
Clinical plans for athletes. To avoid dehydration in most temperate climates, recreational athletes should drink water before, during, and after exercise periods of less than 1 hour with mild or moderate exertion. This includes children and adolescents who play most recreational sports of less than 1 hour in duration. If the weather is particularly hot or humid and in sports such as football where equipment impairs normal heat loss through perspiration, the use of ORT products can be recommended to prevent dehydration. Sports drinks are not recommended because of their high glucose content, and energy drinks should never be used because they contain stimulants that have been associated with cardiovascular symptoms, events, and deaths.19
Recreational and elite athletes engaging in intense or prolonged exercise need aggressive fluid, electrolyte, and carbohydrate replacement. Sports drinks with moderate levels of electrolytes and increased glucose content can be used in these situations. If mild or moderate dehydration develops in adolescent or adult athletes, decreases in total body weight can be used to estimate the fluid deficit. Athletes should adjust their pre-exercise routine to compensate for this fluid deficit if future conditions are similar to those during the dehydration episode, keeping in mind the normal daily requirement of 1.5 to 1.6 L of water for all adults.
PATIENT EDUCATION ON DEHYDRATION AND REPLACEMENT THERAPY
Pharmacists and pharmacy technicians should reinforce several points when counseling patients on the prevention and treatment of dehydration, including the following:
- Continue or reinstate a normal diet (including breastfeeding of infants and young children) as symptoms permit
- Seek medical care if symptoms continue or severe dehydration develops despite treatment
- Monitor infants, young children, and older patients closely for symptoms during replenishment therapy and while any precipitating factors persist (e.g., fever, vomiting, diarrhea, heat, and humidity)
- Reinforce that sports and energy drinks, cola products, and teas should not be used for preventing or treating most cases of dehydration
- Adequate hydration is needed throughout life; drink plenty of clean water each day as part of a healthy lifestyle, and avoid excessive use of caffeine, alcohol, and other lifestyle/dietary factors that can produce dehydration
- Balanced ORT products can be used to prevent dehydration in situations where sufficient clean water is not easily available (e.g., international travel, outdoor exercise without access to water) and for prevention of hangover symptoms following alcohol use
Pharmacists and technicians can also direct patients to several websites and organizations for resources on preventing and treating dehydration (Table 4).31-33,42,43
| Table 4. Resources for obtaining information about preventing and treating dehydration31-33,42,43 |
- Rehydration Project: http://rehydrate.org
- American Academy of Pediatrics, Healthy Children Campaign: https://healthychildren.org/English/Pages/default.aspx
- Product websites: www.pedialyte.com; http://www.enfamil.com/products/solutions-feeding-issues/enfamil-enfalyte; http://www.hydralyte.com
|
SUMMARY
Pharmacists and pharmacy technicians can help consumers navigate available products to prevent and treat dehydration. Water is the only liquid nutrient necessary for human life, and consumption of an adequate amount of clean water is an important part of a healthy lifestyle. Lessons learned during the development of oral therapies for cholera in the 20th century support the current understanding of how dehydration develops and manifests as isotonic, hypertonic, or hypotonic dehydration. Isotonic dehydration is common in several situations: loss of body fluids through sweating, insensible losses from fever or heat exposure, vomiting, diarrhea, and diuresis from caffeine, alcohol, or medication use or diseases such as diabetes insipidus.
Commercially available ORT products are useful for the prevention and treatment of isotonic dehydration. These can be used for replenishment therapy following water deprivation, long-distance travel, and other situations in which hypertonic dehydration has developed. When water is used alone for replacement, the water deficit should be replenished over 48 hours and consumed with a normal diet to avoid hypotonic dehydration from dilution of sodium and other electrolytes. A variety of ORT products, formulations, and flavors are available without a prescription in the U.S. Pharmacy technicians should recognize symptoms suggestive of dehydration and refer consumers exhibiting these symptoms to pharmacists for patient care services, including evaluation, product selection, counseling, and monitoring or follow-up.
REFERENCES
- Jéquier E, Constant F. Water as an essential nutrient: the physiological basis of hydration. Eur J Clin Nutr. 2010;64(2):115-23.
- American College of Emergency Physicians. Dehydration comes on fast and can be fatal. http://www.emergencycareforyou.org/Health-Tips/Dehydration-comes-on-fast-and-can-be-fatal/. Accessed August 2, 2016.
- Ford DM. Fluid, electrolyte, & acid-base disorders & therapy. In: Hay W, Levin M, Deterding R, Abzug M, eds. Current Diagnosis & Treatment: Pediatrics. 22nd ed. New York, NY: McGraw-Hill; 2015:742-751.
- Mayo Clinic. Dehydration. http://www.mayoclinic.org/diseases-conditions/dehydration/basics/symptoms/con-20030056. Accessed August 2, 2016.
- King CK, Glass R, Bresee JS, Duggan C. Managing acute gastroenteritis among children: oral rehydration, maintenance, and nutritional therapy. MMWR Recomm Rep. 2003;52(RR-16):1-16.
- Maughan RJ. Hydration, morbidity, and mortality in vulnerable populations. Nutr Res. 2012;70 Suppl 2:S152-5.
- Keystone JS, Kozarsky PE. Health recommendations for international travel. In: Kasper D, Fauci A, Hauser S, et al, eds. Harrison's Principles of Internal Medicine. 19th ed. New York, NY: McGraw-Hill; 2015. http://accesspharmacy.mhmedical.com/content.aspx?bookid=1130&Sectionid=63652517. Accessed August 2, 2016.
- Bhutta ZA, Das JK, Walker N, et al, for The Lancet Diarrhoea and Pneumonia Interventions Study Group. Interventions to address deaths from childhood pneumonia and diarrhea equitably: what works and at what cost. Lancet. 2013;381(9875):1417-29.
- Das JK, Salam RA, Bhutta ZA. Global burden of childhood diarrhea and interventions. Curr Opin Infect Dis. 2014;27(5):451-8.
- Russo TA, Johnson JR. Diseases caused by gram-negative enteric bacilli. In: Kasper D, Fauci A, Hauser S, et al, eds. Harrison's Principles of Internal Medicine. 19th ed. New York, NY: McGraw-Hill; 2015. http://accesspharmacy.mhmedical.com/content.aspx?bookid=1130§ionid=79735990. Accessed August 2, 2016.
- Roecker A, Bates B, Martin S. Gastrointestinal infections and enterotoxigenic poisonings. In: DiPiro JT, Talbert RL, Yee GC, et al, eds. Pharmacotherapy: A Pathophysiologic Approach. 10th ed. New York: McGraw-Hill; 2016. http://accesspharmacy.mhmedical.com/content.aspx?sectionid=133893751&bookid=1861&jump sectionID=133893849&Resultclick=2#1131967449. Accessed August 2, 2016.
- CaJacob NJ, Cohen MB. Update on diarrhea. Pediatr Rev. 2016;37(8):313-22.
- Waterhouse J, Reilly T, Edwards B. The stress of travel. J Sports Sci. 2004;22(10):946-66.
- Verster JC. The alcohol hangover—a puzzling phenomenon. Alcohol Alcohol. 2008;43(2):124-6.
- Stephens R, Ling J, Heffernan TM, et al. A review of the literature on the cognitive effects of alcohol hangover. Alcohol Alcohol. 2008;43(2):163-70.
- Martin A. Science's best hangover cures. The Wire: News from the Atlantic. December 29, 2011. http://www.thewire.com/entertainment/2011/12/sciences-best-hangover-cures/46786. Accessed August 2, 2016.
- Kelly DG, Nadeau J. Oral rehydration solution: a “low-tech” oft neglected therapy. Nutr Issues Gastroenterol. 2004;28(10):51-62.
- Mount DB. Fluid and electrolyte disturbances. In: Kasper DL, Fauci AS, Hauser SL, et al, eds. Harrison’s principles of internal medicine. 19th ed. New York: McGraw-Hill; 2015. http://accesspharmacy.mhmedical.com/content.aspx?bookid=1130§ionid=79726591. Accessed August 3, 2016.
- American Academy of Pediatrics Committee on Nutrition and the Council on Sports Medicine and Fitness. Sports drinks and energy drinks for children and adolescents: are they appropriate? Pediatrics. 2011;127(6):1182-9.
- Adan A. Cognitive performance and dehydration. J Am Coll Nutr. 2012;31(2):71-8.
- National Institute of Allergy and Infectious Diseases. Cholera. Oral rehydration therapy: a top medical advance of the 20th century. https://www.niaid.nih.gov/topics/cholera/Pages/ort.aspx. Accessed August 2, 2016.
- Fontaine O, Garner P, Bhan MK. Oral rehydration therapy: the simple solution for saving lives. BMJ. 2007;334 Suppl 1:s14.
- Phillips RA. Water and electrolyte losses in cholera. Fed Proc. 1964;23:705-12.
- World Health Organization. Oral rehydration salts: production of the new ORS. Geneva, Switzerland: WHO Document Production Services; 2006.
- World Gastroenterology Organisation global guidelines: acute diarrhea in adults and children: a global perspective. Milwaukee, WI: World Gastroenterology Organisation; February 24, 2012. http://www.guideline.gov/content.aspx?id=47569. Accessed August 2, 2016.
- Kenefick RW, Cheuvront SN. Hydration for recreational sport and physical activity. Nutr Rev. 2012;70 Suppl 2:S137-42.
- Gatorade Sports Science Institute. SSE #97: Hydration assessment of athletes. http://www.gssiweb.org/Article/sse-97-hydration-assessment-of-athletes. Accessed August 2, 2016.
- Canavan A, Arant BS Jr. Diagnosis and management of dehydration in children. Am Fam Phys. 2009;80(7):692-6.
- Steiner MJ, DeWalt DA, Byerley JS. Is this child dehydrated? JAMA. 2004;291(22):2746-54.
- Hooper L, Abdelhamid A, Attreed NJ, et al. Clinical symptoms, signs and tests for identification of impending or current water-loss dehydration in older people. Cochrane Database Syst Rev. 2015;4:CD009647.
- Abbott Global. Pedialyte product information. https://pedialyte.com/. Accessed August 10, 2016.
- Mead Johnson Nutrition. Enfamil product information. http://www.enfamil.com/. Accessed August 10, 2016.
- Hydralyte LLC. Hydralyte product information. http://www.hydralyte.com/. Accessed August 10, 2016.
- The Coca-Cola Company. Powerade product information. http://www.us.powerade.com. Accessed August 10, 2016.
- The Coca-Cola Company. Product facts: ingredient information. http://www.coca-colaproductfacts.com/en/coca-cola-ingredients/#glossary. Accessed August 10, 2016.
- Hoffman MD, Stuempfle KJ. Is sodium supplementation necessary to avoid dehydration during prolonged exercise in the heat? J Strength Cond Res. 2016;30(3):615-20.
- Turner MJ, Avolio AP. Does replacing sodium excreted in sweat attenuate the health benefits of physical activity? Int J Sport Nutr Exerc Metab. 2016;26(4):377-89.
- American Academy of Pediatrics. Diarrhea in babies. https://healthychildren.org/English/ages-stages/baby/diapers-clothing/Pages/Diarrhea-in-Babies.aspx. Accessed August 20, 2016.
- Arvola T, Laiho K, Torkkeli S, et al. Prophylactic Lactobacillus GG reduces antibiotic-associated diarrhea in children with respiratory infections: a randomized study. Pediatrics. 1999;104(5):e64.
- Wingate D, Phillips SF, Lewis DJ, et al. Guidelines for adults on self-medication for the treatment of acute diarrhoea. Aliment Pharmacol Ther. 2001;15(6):773-82.
- Walker PC. Diarrhea. In: Krinsky DL, Ferreri SP, Hemstreet BA, et al, eds. Handbook of Nonprescription Drugs: An Interactive Approach to Self-care. Washington, DC: American Pharmacists Association; 2015: 275-7.
- The Mother and Child Health and Education Trust. Rehydration Project. http://rehydrate.org/. Accessed August 25, 2016.
- American Academy of Pediatrics. Healthychildren.org. https://healthychildren.org/. Accessed August 25, 2016.
Back to Top