
Expired activity
Please go to the PowerPak
homepage and select a course.
Vaccination as a Key Component of Healthy Aging: Focus on Herpes Zoster
ABSTRACT
The U.S. population is aging. This country’s demographic will change in the upcoming decade, and health care providers should be prepared. Disease prevention is imperative as patients age, so immunizations are critical. Elderly patients experience immunosenescence, an aging of the immune system, that leaves them more susceptible to disease and less responsive to vaccines. Modern medicine is trying to keep up with this need through age-appropriate vaccines that use adjuvants, higher doses, and recombinant technology tailored to the aging immune system. Vaccine-preventable diseases (e.g., influenza, pneumococcal disease, herpes zoster) can be detrimental to older individuals’ health, causing ongoing morbidity, decreased quality of life, and even death. Pharmacists are positioned to address vaccine hesitance and promote age-appropriate vaccinations to keep the elderly population healthier.
INTRODUCTION
The United States (U.S.) is approaching an important demographic milestone. In 2030, all baby boomers—those born between 1946 and 1964—will be older than 65. Within just a few decades, older people will outnumber children for the first time in history.1 The need is greater than ever for healthcare professionals to understand the elderly population’s unique needs. Vaccine-preventable diseases (e.g., influenza, pneumococcal disease, herpes zoster) are an area of concern, as they affect older patients disproportionately.
In the Middle Ages, people sometimes referred to influenza as “the kind illness” for its typically mild clinical course. However, each year, influenza causes seasonal epidemics of serious illness and death throughout the world. Signs and symptoms—fever, cough, nasal congestion, body aches, and fatigue—start abruptly about 2 days after exposure and most patients recover in about 1 week. Others may develop life-threatening complications like pneumonia and influenza is particularly fatal to the elderly population.2 About 67% of elderly patients with influenza become at least temporarily housebound, and 25% become bedbound. Influenza is also one of the leading causes of outbreaks in long-term care facilities. These outbreaks affect 33% of a facility’s population on average and mortality rates can reach 55% in long-term care residents who contract influenza.3
Pneumococcal diseases (PD)—infections caused by Streptococcus pneumoniae or pneumococcus—are divided into non-invasive and invasive disease. Non-invasive PD includes sinusitis, acute otitis media, and community-acquired pneumonia (CAP). Invasive PD involves infection of a normally sterile site, including blood (pneumococcal bacteremia) or cerebrospinal fluid (pneumococcal meningitis).4,5 PD rates have always been higher in the very young and the very old. Pneumococcal pneumonia is the most common PD in the elderly; comorbid disease, impaired mucociliary clearance, and a waning immune system leave them at an increased risk.5 An estimated 915,900 cases of CAP occur annually among senior in the U.S., and about 1 of every 20 people 85 years or older will have a new CAP episode each year. Pneumonia is also a leading cause of death among older adults. In the U.S., about 600,000 hospitalizations for CAP and 59,000 deaths attributed to pneumonia and influenza occur among seniors yearly.6
About one-third of people in the U.S. will develop herpes zoster, also known as shingles, in their lifetime.7 Individuals previously infected with chicken pox may develop shingles later in life. Following initial varicella (chicken pox) infection, the virus establishes permanent latent infection in dorsal root and cranial nerve ganglia of the spinal cord. Years to decades later, the virus may reactivate and spread through peripheral nerves to the skin, causing pain and a unilateral vesicular rash. Herpes zoster infects about 1 million people yearly in the U.S., and the risk of contracting it increases with age.7 In fact, age is its most important risk factor. Incidence of herpes zoster more than doubles from 5 cases per 1,000 population in adults aged 50 to 59 to 11 cases per 1,000 population in people aged 80 years and older. Approximately half of people who live 85 years or more will experience shingles, and about 80% to 85% of postherpetic neuralgia (PHN)—herpes zoster’s most debilitating complication—occurs in patients aged 50 years or older.8
CASE STUDY: Sally, a 73-year-old retired factory worker, tells you that she cut herself on a rusty gardening tool, and asks for a tetanus shot. When you ask her what other vaccines she has received, she says that she had her last tetanus shot in her 40s when she was working. She has had no other vaccinations except perhaps a flu shot many years ago. What vaccines does she need?
Current Vaccine Recommendations
The U.S. Centers for Disease Control and Prevention (CDC) and the Advisory Committee on Immunization Practices (ACIP) recommend vaccination against all 3 of these infections in the aging population. All persons aged 6 months or older should receive the seasonal influenza vaccine yearly, but ACIP advises providers to emphasize high-risk populations, including individuals 50 years and older. This recommendation also extends to household contacts and caregivers of people 50 years and older.9 High-dose trivalent inactivated influenza vaccine (IIV3)—to be discussed in detail later—has demonstrated superior efficacy over standard-dose IIV3 and may provide better protection than standard-dose IIV3 in patients 65 years and older. However, ACIP does not recommend delaying vaccination if a high-dose product is unavailable.9
Two pneumococcal vaccines exist: 23-valent pneumococcal polysaccharide vaccine (PPSV23) and 13-valent pneumococcal conjugate vaccine (PCV13). CDC recommends 1 dose of PPSV23 for all adults 65 years and older, regardless of previous pneumococcal vaccine history. Once a dose of PPSV23 is administered at age 65 years or older, no additional doses of PPSV23 should be given. Providers should consider PCV13 administration on a case-by-case basis in this population, including patients at increased risk of exposure to PCV13 serotypes (e.g., living in a long-term care facility or nursing home). People with underlying medical conditions (e.g., chronic heart, lung or renal disease, diabetes, alcoholism, cigarette smoking) should also receive the PCV13 vaccine. If the patient has not received PCV13 previously and patient and provider decide jointly that PCV13 is to be given, the following should be considered10:
- for those who have not received any pneumococcal vaccines, or those with unknown vaccination history
- administer 1 dose of PCV13
- administer 1 dose of PPSV23 at least 1 year later
- for those who have previously received 1 dose of PPSV23 at 65 years of age or older and no doses of PCV13
- administer 1 dose of PCV13 at least 1 year after the dose of PPSV23 was given
When both are indicated, providers should administer PCV13 before PPSV23 whenever possible. Also, clinicians should not administer both vaccines during the same office visit.10
In the U.S., health authorities have licensed and recommended 2 shingles vaccines: zoster vaccine live (ZVL) since 2006 and recombinant zoster vaccine (RZV) since 2017. RZV is recommended as the preferred shingles vaccine. In fact, as of July 1, 2020, ZVL is no longer sold in the U.S. Pharmacies and clinics with remaining ZVL in stock can use it until it expires or until November 18, 2020, whichever comes first.11 RZV vaccination is recommended for12
- immunocompetent adults aged 50 years or older
- immunocompetent adults previously vaccinated with ZVL
The efficacy of RZV for prevention of herpes zoster is exceptional12:
- 6% for patients aged 50 to 59
- 4% for patients aged 60 to 69
- 3% for patients aged 70 or older
- 6% in the first year, 84.7% for the following 3 years
RZV also shows 91.2% efficacy in prevention of PHN in adults 50 years or older and 88.8% in those 70 years or older.12 Clearly, the importance of RZV vaccination in adults 50 years and older cannot be understated.
Vaccinating against these 3 diseases can lead to a reduction in comorbid conditions (e.g., cardiovascular and cerebrovascular disease), diminished long-term effects of the infections, and reduced hospital admissions. It can also prevent premature death. Of note, ACIP indicates that these vaccines can be co-administered (except PCV13 and PPSV23), so pharmacists should encourage patients not to delay vaccination against any of these diseases.9
IMMUNE-RELATED CHANGES IN THE ELDERLY
Elderly adults are more susceptible to infections from a variety of diseases. When infected, those diseases are also more severe in older patients compared to younger patients due to immune-related changes. Immunosenescence also affects vaccine response in elderly adults, and age-specific vaccines can help.
Immunosenescence
Aging causes immune system remodeling, which leads to a progressive decline in immune responses, referred to as immunosenescence. It decreases protection from infection and decreases ability to respond to new and emerging pathogens. Proper defense from infectious diseases requires cooperation from both branches of the immune system, innate and adaptive, to produce a highly coordinated response.
The innate immune system consists of neutrophils, macrophages, dendritic cells, and natural killer cells. These are the “first responders” to infection. In older adults, these cells exhibit delayed migratory ability, impaired phagocytosis, impaired cytotoxicity, reduced cytokine secretion, altered antigen presentation, and altered signaling patterns, summarized in Table 1.13
| Table 1. Effects of Immunosenescence on the Innate and Adaptive Immune Systems |
| Cell Type |
Function |
Effects of Aging |
| Innate Immune System |
|
Neutrophils
|
· Prevent the spread of invading pathogens
|
· Reduced chemotaxis (movement toward pathogens)
· Reduced phagocytosis (ingestion) of microbes
· Reduced generation of reactive oxygen species for cell death
|
|
Macrophages
|
· Detection, phagocytosis, and destruction of invading organisms
· Present antigens to T cells to activate adaptive immune system
|
· Decreased macrophages in the bone marrow
· Reduced chemotaxis and phagocytosis
|
|
Dendritic cells
|
· Sequester antigens, migrate to secondary lymphoid organs, and present antigens to the adaptive immune system
|
· Decreased expression
· Reduced migratory response
· Reduced uptake of antigens
|
|
Natural killer cells
|
· Destroy physiologically stressed cells (e.g., tumor cells) and virus-infected cells
|
· Decreased bone marrow production
· Reduced cytotoxicity
· Decreased production of interleukins (immune response regulators)
· Altered T cell proliferation
|
| Adaptive Immune System |
|
B cells
|
· Produce antibodies, which lock to the surface of an invading cell to mark it for destruction by other immune cells
|
· Decreased naive B cells (reduced response to new pathogens)
· Increased memory B cells (respond only to known pathogens)
|
|
T cells
|
· Destroy infected cells
· Signal to other immune cells to participate in immune response
|
· Decreased production of naive T cells by the thymus
· Increased memory T cells
|
The adaptive immune system (also referred to as the acquired immune system) also suffers from the effects of aging. This branch consists of specialized, systemic lymphocytes—also known as B cells and T cells—that eliminate pathogens by preventing their replication. Older adults have decreased bone marrow density, shifting the typical balance of B cells. Younger individuals have many naive B cells and fewer memory B cells; aging adults have the opposite. Additionally, the thymus, which is involved in T cell production, regresses in the elderly. This leads to decreased epithelial cells (resulting in overall diminished tissue and cellular regeneration) and increased infiltrating adipocytes (altering immune cell activation).15 Older individuals respond to new infections and vaccines with novel antigens less effectively.
The aging process is also associated with development of chronic, low-grade, sterile inflammation, referred to as inflammaging. It causes a major alteration in intercellular communication, and it is implicated in pathogenesis of conditions including osteoporosis, atherosclerosis, Alzheimer’s disease, and type 2 diabetes mellitus.16 Various mechanisms have been implicated in inflammaging16:
- Chronic stimulation of the immune system by viruses such as cytomegalovirus (a common virus retained by the body for life once infected, but typically causing no illness)
- Decreased adaptive immune system function and loss of ability to contain viral infections, thereby extending duration of the innate immune system response
- Translocation of microbial products from the gut into the circulation due to reduced integrity of the intestinal epithelial barrier
- Increased adipose tissue accumulation, which increases levels of inflammatory cytokines
In short, inflammaging causes a shift in the immune environment from anti-inflammatory in infancy to pro-inflammatory in old age.16
CASE STUDY: Richie has just turned 70, and he asks for a shingles shot. You have 2 in stock: the older ZVL and the newer RZV. Make the case for Richie to receive the newer vaccine.
Decreased Vaccine Effectiveness
Vaccination is modern preventive medicine’s main strategy. It establishes protective immunity among the population to prevent, and sometimes eradicate, diseases. In older adults, however, primary vaccine responses are weaker, often failing to produce long-term protective immunity and leaving them susceptible to disease.
Changes in the adaptive immune system are implicated in lower vaccine effectiveness in older individuals. As mentioned, the balance of naive- and memory-B cells in the elderly shifts so that terminally-differentiated memory cells predominate.14 Memory cells only recognize antigens from previous infections, so they do not protect an individual from new diseases or provide immunity to new pathogens. This leaves the elderly more susceptible to new disease and reduces response to vaccines containing novel antigens.
Evidence of this phenomenon is reflected in vaccine efficacy rates. For example, influenza vaccination has been estimated to protect between 70% to 90% of children and adults, but protection estimates fall to 30% to 50% in patients aged 65 and older.15 As noted, the elderly experience impaired antigen processing and presentation, which diminishes immune response. Migration of antigen presenting cells, antigen presentation by dendritic cells, and cytokine production are also affected. This leads to poor antibody recruitment and decreases IgA and IgG concentrations, delays peak titers, and rapidly lowers antibody concentrations. Elderly patients also experience a shift from proinflammatory cytokines to more anti-inflammatory cytokines, which may correlate to reduced cytotoxic T cell response and impaired vaccine response.17
Tailoring Vaccines to the Elderly
Decreased vaccine responsiveness calls for adaptations to vaccines to tailor them to the aging immune system and improve immune response in the elderly. Vaccine manufacturers can use 3 approaches: (1) high-dose formulations, (2) formulations with adjuvants, and (3) recombinant vaccines.
The high-dose influenza vaccine contains 4 times the amount of antigen compared to the standard-dose, and is associated with a stronger immune response and better effectiveness in older patients. Notably, this response still does not achieve the magnitude of that induced by the standard dose in younger adults.15
Adjuvants are substances added to vaccine formulations that can enhance and skew immune responses. They increase antigen immunogenicity (ability to provoke a response).15,18 They can increase the adaptive immune system’s response dramatically by activating the innate response. Collectively, the actions may15
- enhance the immune response’s speed and magnitude
- reduce the dose of antigen and/or vaccinations needed
- increase cross-protection
- reduce non-responsiveness in special populations, such as the elderly
Independent of immune response, adjuvants can also increase vaccine stability so antigens are less susceptible to degradation during storage or upon injection.18 The key to developing adjuvants for use in vaccines targeted to the elderly is that the substances should optimally balance immune stimulation and the inflammatory status of the aging immune system. That is, researchers should consider the presence of low-grade baseline inflammation (inflammaging) when adding additional inflammatory activity to a vaccine.15
Research has indicated 3 adjuvants are helpful in vaccines for the elderly: MF59 and AS03 in influenza vaccines and AS01 in the recombinant herpes zoster vaccine. First used in 1997, MF59 is an oil-in-water emulsion composed of squalene and surfactants (Tween 80 and Span85).15 Its mechanism is poorly understood, but it is safe and highly potent. It induces recruitment and activation of cells at the injection site, which stimulates expression of several immunostimulatory cytokines that favor antigen uptake by antigen-presenting cells and transport of the antigen to draining lymph nodes.15,18 MF59 also influences both the quantity and quality of anti-influenza antibodies, therefore increasing the breadth of antibody response.15
AS01 and AS03 belong to the adjuvant family called “Adjuvant Systems” (AS). AS are obtained by combining immunostimulatory molecules with classic adjuvants (e.g., aluminum salts, liposomes, oil-in-water emulsions) and are designed to provide better and broader protection than standard formulations. AS03 contains squalene and alpha-tocopherol. Alpha-tocopherol is a major bioavailable form of vitamin E, which has immunostimulant and anti-oxidant properties. It must be included in AS03 to induce a high antibody response.15,18 AS03 strongly induces upregulation of genes encoding inflammatory cytokines and chemokines in the lymph nodes.
AS01 is a liposome-based adjuvant system that contains 2 immunostimulant molecules: MPL and QS-21. AS01 activates the innate immune response rapidly and transiently in the injected muscle and the draining lymph node.15,19 This increases the number of activated antigen-presenting cells. Therefore, inclusion of AS01 in the recombinant herpes zoster vaccine creates a stronger T cell response when compared to a vaccine without it.15,19
Older patients who received the original herpes zoster vaccine, ZVL, experienced waning efficacy. Clinical trials indicated that ZVL’s efficacy for herpes zoster prevention in individuals 50 to 59 years old was 70%. They also found that efficacy declined with age from 64% in people 60 to 69 years old to 18% in those 80 years or older. ZVL’s efficacy also decreased over time, from 62% in the first year after vaccination to approximately 40% within 5 years.20
Researchers used recombinant vaccine technology to create RZV and overcome immunosenescence and address the need for a better vaccine. Recombinant vaccines use only specific pieces of the pathogen, which gives them a strong, targeted immune response. RZV uses a recombinant glycoprotein E (gE) subunit combined with the AS01 adjuvant system. Researchers selected gE as the vaccine antigen because it is the most abundant glycoprotein expressed by cells infected with varicella zoster virus. It also induces both neutralizing antibody and CD4 T-cell responses.20
Phase 3 efficacy trials, ZOE-50 and ZOE-70, assessed RZV’s efficacy in adults 50 years and older and 70 years and older, respectively. Two doses of RZV administered intramuscularly 2 months apart demonstrated age-dependent efficacy (stated above) with an acceptable safety profile.12,20 Efficacy also remained high at 88% over the 4-year duration of the ZOE-70 trial. Researchers concluded that RZV can overcome immunosenescence to provide enduring herpes zoster protection.20 A limitation to recombinant vaccines is the need for multiple shots—or booster shots—for ongoing protection. Efficacy of a single RZV dose has not been studied, but exploratory, post-hoc analyses have confirmed that the second dose is necessary. These analyses estimated that the efficacy of RZV drops to 90.8% in people 50 years or older and 69.5% in those 70 years who receive only 1 dose.21
THE ELDERLY ARE NOT GETTING VACCINATED
Older adults are clearly more susceptible to disease, but they are also susceptible to vaccine hesitance (avoiding vaccination in spite of available vaccines). Low vaccine coverage is worldwide, which led the World Health Organization to identify vaccine hesitance as a top 10 threat to global health in 2019.22 Vaccination rates among the elderly are especially inadequate. In 2016, ACIP reported that coverage rates for adults 60 years and older were 70.4%, 66.9%, and 33.4% for influenza, pneumococcal disease, and herpes zoster, respectively.23
Consequences of Missed Vaccinations
Diseases with low vaccination coverage in older patients, such as herpes zoster, should be an important focus, since a large number of unvaccinated patients are at risk for development of complications. Influenza remains the leading cause of infectious death in the elderly. Seasonal influenza outbreaks cause approximately 36,000 deaths and 226,000 hospitalizations yearly, and more than 90% of that mortality is incurred by people 65 and older.24 Underlying comorbid conditions, close living quarters, and shared caregivers also leave nursing home residents at increased exposure risk. Influenza can also cause significant functional decline in those who are hospitalized. Over one-third of hospitalized patients 70 years or older leave the hospital more disabled than when they arrived. Elderly patients are more likely to experience frequent and prolonged hospitalizations due to influenza, and therefore suffer from significant functional loss.24 Other influenza complications are shown in Table 2. Vaccination has proven helpful; a systematic review found a 26% reduction in hospitalization from influenza and pneumonia and a 42% reduction in all-cause mortality among community-dwelling elderly. These numbers rose to 46% and 60% respectively in nursing home residents.24 Repeated vaccinations increased these protective effects, while mortality risk rose to 40% above baseline if annual vaccination was interrupted.24
| Table 2. Complications of Influenza, Pneumococcal Disease, and Herpes Zoster in the Elderly24-26 |
| Disease |
Complications |
| Influenza |
Cardiovascular morbidity (heart disease and stroke)
Exacerbation of chronic pulmonary disease (e.g., asthma, chronic bronchitis)
Mixed viral and bacterial pneumonia |
Hospitalization
Death
Rare: myositis, rhabdomyolysis, encephalitis |
| Pneumococcal Disease |
Meningitis
Bacteremia
Empyema (infection of space between membranes surrounding lungs and chest cavity)
Pericarditis (inflammation of sac surrounding the heart)
Endobronchial obstruction (blockage of airway that allows air into the lungs) |
Atelectasis (lung collapse)
Lung abscess (collection of pus)
Brain damage
Hearing loss
Sepsis
Hospitalization
Death |
| Herpes Zoster |
Postherpetic neuralgia
Ocular manifestations (e.g., glaucoma, optic neuritis, blindness)
Pneumonia
Hearing problems
Encephalitis (brain inflammation) |
Meningitis
Cranial neuritis
Visceral complications
Hospitalization
Death |
Pneumococcal disease can be mild, causing only a sinus or ear infection, but older adults are most likely to suffer from serious complications or death. The chance of death from pneumococcal meningitis, bacteremia, or pneumonia is higher for elderly patients.25 About 24,000 cases of invasive PD occur in the U.S. yearly among adults 50 years and older, resulting in 4,500 deaths.27 Proper vaccination against PD shows a 56% reduction in the risk of invasive PD, highlighting a need for vaccination among the elderly.27 As highlighted in Table 2, pneumococcal disease comes with a plethora of possible complications affecting the lungs and heart, in addition to sepsis and death.
Patients may perceive shingles—which presents dermatologically—as “less serious” than respiratory disorders like influenza or pneumonia. However, complications of the disease are severe. PHN is the most common complication of shingles. PHN is defined as pain distributed to a dermatomal area (an area of skin supplied by cutaneous branches of a single cranial or spinal nerve) that is sustained for at least 90 days after the shingles rash.28 It causes severe, debilitating pain that patients describe as burning or electric shock-like. Patients can also experience allodynia, which can be the most debilitating. Allodynia occurs when normal tactile experiences (e.g., clothing, wind, etc.) cause severe pain. This can continue for weeks, months, or rarely even years, affecting physical functioning, psychological well-being, and quality of life. Patients with PHN are at risk of anxiety, depression, weight loss, sleep disturbance, and social isolation and may have difficulty with activities of daily living.26
PHN affects about 20% of herpes zoster patients, but elderly patients are disproportionately affected, as 80% of cases occur in people 50 years or older.28 Although some patients’ symptoms resolve completely after several years, others continue to take medications for PHN indefinitely. PHN can be especially debilitating in frail, older patients; .29 Depending on the nerve location of herpes zoster’s reactivation, it can cause other neurologic complications, including those in Table 2. As mentioned, vaccination prevents PHN significantly in the older population.12 Pharmacists should encourage patients 50 years and older to receive RZV to reduce the risk of complications, even if they perceive shingles as “less severe” than other diseases.
CASE STUDY: After reviewing a 62-year-old male patient’s vaccination history, a consultant pharmacist discovers that the patient has never received the herpes zoster vaccine. When the pharmacist recommends vaccination to the patient, the patient states that he does not need it. Provide evidence to support the need for vaccination in this patient and address any barriers that may exist.
Barriers to Appropriate Vaccination
Educational barriers and misconceptions get in the way of vaccine adherence in older patients. As stated, older adults are susceptible to vaccine hesitancy and vaccine rates among the elderly are inadequate. Vaccine administration requires more decisional conflict than disease treatment, as it requires intervention in an otherwise healthy individual. Some vaccines-preventable diseases are rare enough that individuals may not understand their seriousness (e.g., invasive PD), while others are so common than they generate complacency (e.g., influenza). Additionally, as vaccines become more effective and reduce disease occurrence, infrequent encounters with the disappearing disease makes vaccination seem unnecessary. This fosters complacency and encourages skipped vaccines.30
Older adults may also be unaware of the need for vaccination. A 2017 survey addressed influenza vaccination beliefs and practices in patients 65 years and older.31 Only about one-half of the 200 participants thought the influenza vaccine was very effective or very safe, while the other half were less certain. One third of respondents had specific concerns about the vaccine with the following themes31:
- flu vaccine causes side effects
- flu vaccine is not effective
- flu vaccine components are harmful
- flu vaccination is not necessary
- vaccine experiences of friends and family
The most common concern (11.5% of participants) was that the vaccine causes the flu or flu-like illness.
A 2013 survey of 403 primary care patients 60 years and older found that only 7.7% of them had received the herpes zoster vaccine.32 Interestingly, about 70% of them indicated they hadn’t even heard of it. Conversely, of the patients who had already received the vaccine, 48% said it was recommended by a health care provider. This underscores how important it is for pharmacists and other health care professionals to ensure their older patients are aware of available vaccines and recommend them. Some other reasons for herpes zoster vaccine avoidance included32
- do not think I will develop shingles
- physician did not recommend it
- afraid of the side effects
- financial reasons
- do not believe in vaccines in general
- do not think shingles will cause significant or lasting illness
- do not think the vaccine works
Many of these barriers can be overcome with education. Pharmacists should be prepared to educate patients about the increased risk of shingles with age, possible lasting effects of shingles (i.e., PHN), the benefits of vaccination, and adverse effect management.
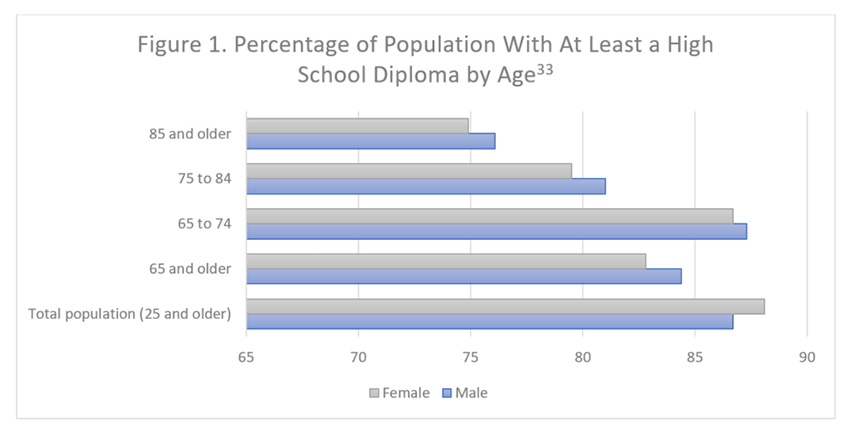
Pharmacists should be cautious, however, to present vaccine-related information in an easy-to-understand way. In 2016, the U.S. Census Bureau concluded that the older population is less likely to have a high school diploma than the total population (Figure 1)33 This may make understanding the science behind vaccines more difficult and increases the likelihood that their necessity will be underestimated.
Cost is another important barrier. This is not typically an issue for the influenza vaccine, as Medicare Part B covers the shot yearly at no cost to the patient. The same benefits cover the pneumococcal vaccine at no out-of-pocket cost. The same cannot be said, however, for the herpes zoster vaccine. All Medicare Part D drug plans or Medicare Advantage plans that include prescription coverage usually cover the shingles vaccine, but not in its entirety. Depending on the plan, patients may incur an out-of-pocket cost as a copayment (fixed dollar amount) or coinsurance (percentage of the vaccine’s cost).34 CDC reports that as of September 1, 2020, the cost of RZV is $151.41 per dose.35 Therefore, costs can be significant for patients who have not met the deductible or have an especially high coinsurance. Some plans also require patients to receive the vaccine at a physician’s office rather than a pharmacy. Pharmacists should be sure to work with patients to find an in-network pharmacy or provider’s office to administer the vaccine if it is not covered at their location.34
Pharmacists should also be prepared to emphasize risk versus benefit when discussing vaccine costs. The U.S. Department of Health and Human Services estimates that the average cost of shingles treatment is $525 per person.36 A 2008 study found that patients on Medicare who had persisting pain due to PHN spent nearly $2700 more annually than those who did not develop PHN. This number increased to more than $4900 for commercially-insured patients.37 . Patients should consider these added costs, along with significant negative impact on quality of life, when making a decision to avoid the shingles vaccine.
Remaining barriers to vaccine administration are largely due to convenience. Influenza vaccination is required on an annual basis, while and herpes zoster vaccines both require 2 doses. n. A 2018 survey of older adults found that provider recommendations promoting shingle vaccination positively influenced willingness to be vaccinated.38 Highlighted in particular was the need to provide patients with efficacy rates to encourage completion of the 2-dose RZV series. Researchers asked participants: “All other things being equal, if you are offered a shingles vaccine that is 97.2% protective and requires two doses gives 2 months apart (vaccine #1) or a shingles vaccine that is 51.3% protective and requires one dose (vaccine #2), which vaccine would you choose?” An overwhelming majority (88.2%) of patients indicated that they would choose vaccine #1.38 This indicates that providing patients with basic evidentiary information about vaccines can help overcome the barrier of multiple-dose requirements.
CASE STUDY: Richie had his first dose of RZV 5 months ago. He is due for a second dose. What are the best ways to ensure he receives that second dose?
Strategies for Vaccine Promotion in the Elderly
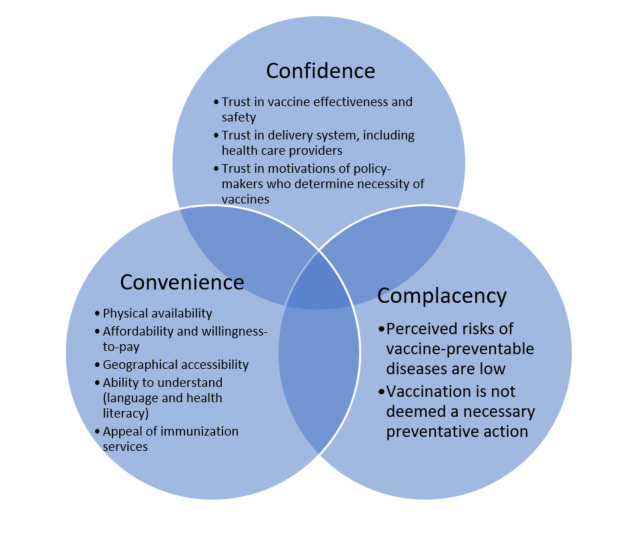
The World Health Organization describes vaccination barriers with the “3 Cs” model, shown in Figure 2, highlighting 3 categories: confidence, complacency, and convenience.39 To accept vaccinations, patients must have affordable and easy access, be confident in the health care provider’s knowledge and skills, and be aware of all vaccinations recommended for their age group. Pharmacists are perfectly positioned to address these barriers to vaccine administration40:
- Confidence: Pharmacists are one of the most trusted health care professionals in the U.S, and they have been ranked the second most highly trusted health-care professional to deliver vaccinations after physicians. As patient educators, pharmacists can promote vaccine coverage by increasing patients’ confidence in vaccines. Pharmacists maintain competency through continuing education (such as this!) and are well prepared to address questions and concerns about vaccine indications, efficacy, and safety.
- Convenience: Pharmacists are the most readily accessible health care providers in the U.S. and patients see a pharmacist up to 10 times more frequently than their primary care provider. Surveys have found that the majority of Americans prefer visiting a pharmacy for vaccinations as opposed to visiting a primary care office. Frequent pharmacy contact provides a supreme opportunity to improve vaccination rates.
- Complacency: National surveys indicate that older adults tend to be aware of some vaccinations, including influenza (97%) and pneumococcal (87%), but less aware of others, including herpes zoster (73%). Pharmacists are poised to close this awareness gap by (1) screening patient history for vaccination needs, (2) counseling patients on vaccine guidelines, recommendations, and safety, (3) managing inventories to ensure vaccine stock levels are appropriate, and (4) community outreach efforts.
Figure 2. World Health Organization “3 Cs” Model39
Another conversational strategy that pharmacists can turn to for guidance is CDC’s “SHARE” model41:
- SHARE specific reasons why a recommended vaccine is right for a patient, referencing their age, health status, lifestyle, occupation, or other risk factors
- HIGHLIGHT positive vaccine experiences, personal or otherwise, to reinforce benefits and confidence in vaccination
- ADDRESS any questions and concerns the patient has, including safety, adverse effects, and vaccine effectiveness in plain, understandable language
- REMIND patients that vaccines protect them and their loved ones from common and serious diseases
- EXPLAIN potential costs of contracting the disease, rather than the vaccine, including serious health consequences, lost time from work or enjoyable activities, and financial costs
In the case of herpes zoster vaccination, pharmacists should be vigilant to ensure patients receive both doses. Research indicates that a simple reminder call can make a big difference. A 2019 study involved pharmacy interns calling more than 1000 patients who received an initial dose of RZV to remind them that the second dose was coming due.42 Results showed that 92% of those patients who spoke directly with a pharmacy intern received the second dose, compared with 87% of those who had no contact. Additionally, RZV’s manufacturer offers a website reminder service for patients; it will remind them that their next dose is due by voice, email, and/or text (visit https://www.shingrix.com/2nd-dose-reminder.html). Pharmacists should offer this service to patients upon first-dose administration.
Of note, CDC recognizes that some patients may unintentionally miss the 2- to 6-month window for second-dose administration and offers guidance43:
- If more than 6 months have passed since the first RZV dose, administer the second dose as soon as possible. It is not necessary to restart the vaccine series.
- If the second dose is given less than 4 weeks after the first, the second dose is invalid. Administer an additional dose 2 months after the invalid dose (4 weeks at minimum).
CONCLUSION
The U.S. population is aging and will shift this country’s demographic significantly in the upcoming decade. Elderly individuals undergo immunosenescence with age, leaving them more susceptible to disease and less responsive to vaccinations. Age-appropriate vaccine advancements to counteract immunosenescence are becoming more common, including high-dose, recombinant, and adjuvant formulations. Pharmacists are perfectly poised to address vaccine hesitance, promote age-appropriate vaccinations, and keep the elderly population healthier.
RESOURCES
ACIP Vaccine Schedules (via CDC website)
Information on age-appropriate vaccinations indicated in older adults |
https://www.cdc.gov/vaccines/hcp/acip-recs/index.html |
National Council on Aging
Information on age-appropriate vaccinations in older adults, including what Medicare pays for |
https://www.ncoa.org/ |
Herpes Zoster Vaccine—Second Dose Reminder
Set up a reminder for older patients who may not remember to return for a second RZV dose |
https://www.shingrix.com/2nd-dose-reminder.html |
References
- United States Census Bureau. Older people projected to outnumber children for the first time in U.S. history. Accessed at: https://www.census.gov/newsroom/press-releases/2018/cb18-41-population-projections.html. Published March 13, 2018. Accessed July 15, 2020.
- Gasparini R, Amicizia D, Lai PL, Panatto D. Clinical and socioeconomic impact of seasonal and pandemic influenza in adults and the elderly. Hum Vaccin Immunother. 2012;8(1):21-28.
- Talbot HK. Influenza in older adults. Infect Dis Clin North Am. 2017;31(4):757-766.
- Centers for Disease Control and Prevention. Pneumococcal disease: surveillance and reporting. Accessed at: https://www.cdc.gov/pneumococcal/surveillance.html. Updated September 2017. Accessed July 15, 2020.
- Drijkoningen JJ, Rohde GG. Pneumococcal infection in adults: burden of disease. Clin Microbiol Infect. 2014;20 Suppl 5:45-51.
- Jackson ML, Neuzil KM, Thompson WW, et al. The burden of community-acquired pneumonia in seniors: results of a population-based study. Clin Infect Dis. 2004;39(11):1642-1650.
- Centers for Disease Control and Prevention. Varicella (chickenpox) and herpes zoster (shingles): overview of VZV disease and vaccination for healthcare professionals. Accessed at: https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5705a1.htm. Published June 2008. Accessed July 15, 2020.
- Centers for Disease Control and Prevention. Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP). Accessed at: https://www.cdc.gov/vaccines/vpd-vac/shingles/downloads/VZV_clinical_slideset_Jul2010.pdf. Updated August 2013. Accessed July 15, 2020.
- Centers for Disease Control and Prevention. Influenza (flu): 2019-20 summary of recommendations. Accessed at: https://www.cdc.gov/flu/professionals/acip/summary/summary-recommendations.htm. Updated August 2019. Accessed July 15, 2020.
- Immunization Action Coalition. Ask the experts: pneumococcal vaccines (PCV13 and PPSV23). Accessed at: https://www.immunize.org/askexperts/experts_pneumococcal_vaccines.asp. Updated July 2020. Accessed August 1, 2020.
- Centers for Disease Control and Prevention. Vaccines and preventable diseases: what everyone should know about shingles vaccines. Accessed at: https://www.cdc.gov/vaccines/vpd/shingles/public/index.html. Updated May 2018. Accessed August 1, 2020.
- Dooling KL, Guo A, Patel M, et al. Recommendations of the advisory committee on immunization practices for use of herpes zoster vaccines. MMWR Morb Mortal Wkly Rep. 2018;67(3):103-108.
- Coll PP, Costello VW, Kuchel GA, et al. The prevention of infections in older adults: vaccination. J Am Geriatr Soc. 2020;68(1):207-214.
- Mahbub S, Brubaker AL, Kovacs EJ. Aging of the innate immune system: an update. Curr Immunol Rev. 2011;7(1):104-115.
- Ciabattini A, Nardini C, Santoro F, et al. Vaccination in the elderly: the challenge of immune changes with aging. Semin Immunol. 2018;40:83-94.
- Sadighi Akha AA. Aging and the immune system: an overview. J Immunol Methods. 2018;463:21-26.
- Smetana J, Chlibek R, Shaw J, et al. Influenza vaccination in the elderly. Hum Vaccin Immunother. 2018;14(3):540-549.
- Bastola R, Noh G, Keum T, et al. Vaccine adjuvants: smart components to boost the immune system. Arch Pharm Res. 2017;40(11):1238-1248.
- Lecrenier N, Beukelaers P, Colindres R, et al. Development of adjuvanted recombinant zoster vaccine and its implications for shingles prevention. Expert Rev Vaccines. 2018;17(7):619-634.
- Cunningham AL, Heineman TC, Lal H, et al. Immune responses to a recombinant glycoprotein E herpes zoster vaccine in adults aged 50 years or older. J Infect Dis. 2018;217(11):1750-1760.
- GlakoSmithKline. Vaccine efficacy after one dose of Shingrix in adults ≥ 50 years of age. Accessed at: https://www.publichealthmdc.com/documents/Efficacy%20After%20One%20Dose%20i.pdf. Accessed July 15, 2020.
- World Health Organization. Ten threats to global health in 2019. Accessed at: https://www.who.int/emergencies/ten-threats-to-global-health-in-2019. Accessed August 1, 2020.
- Centers for Disease Control and Prevention. Vaccination coverage among adults in the United States, National Health Interview Survey, 2016. Accessed at: https://www.cdc.gov/vaccines/imz-managers/coverage/adultvaxview/pubs-resources/NHIS-2016.html. Updated February 2018. Accessed September 9, 2020.
- Pop-Vicas A, Gravenstein S. Influenza in the elderly: a mini-review. Gerontology. 2011;57(5):397-404.
- Centers for Disease Control and Prevention. Pneumococcal disease: symptoms and complications. Accessed at: https://www.cdc.gov/pneumococcal/about/symptoms-complications.html. Updated September 2017. Accessed August 1, 2020.
- John AR, Canaday DH. Herpes zoster in the older adult. Infect Dis Clin North Am. 2017;31(4):811-826.
- Jackson LA, Janoff EN. Pneumococcal vaccination of elderly adults: new paradigms for protection. Clin Infect Dis. 2008;47(10):1328-1338.
- McElhaney JE, Verschoor C, Pawelec G. Zoster Vaccination in Older Adults: Efficacy and Public Health Implications. J Gerontol A Biol Sci Med Sci. 2019;74(8):1239-1243.
- Saguil A, Kane S, Mercado M, Lauters R. Herpes zoster and postherpetic neuralgia: prevention and management. Am Fam Physician. 2017;96(10):656-663.
- Jacobson RM, St Sauver JL, Finney Rutten LJ. Vaccine hesitancy. Mayo Clin Proc. 2015;90(11):1562-1568.
- Rikin S, Scott V, Shea S, et al. Influenza vaccination beliefs and practices in elderly primary care patients. J Community Health. 2018;43(1):201-206.
- Joon Lee T, Hayes S, Cummings DM, et al. Herpes zoster knowledge, prevalence, and vaccination rate by race. J Am Board Fam Med. 2013;26(1):45-51.
- United States Census Bureau. The population 65 years and older in the United States: 2016. Accessed at: https://www.census.gov/content/dam/Census/library/publications/2018/acs/ACS-38.pdf. Published October 2018. Accessed July 15, 2020.
- National Council on Aging. Healthy aging in winter and beyond: 4 important vaccines for seniors covered by Medicare. Accessed at: https://www.ncoa.org/blog/4-important-vaccines-seniors-covered-medicare/. Published November 2017. Accessed August 1, 2020.
- Centers for Disease Control and Prevention. CDC vaccine price list. Accessed at: https://www.cdc.gov/vaccines/programs/vfc/awardees/vaccine-management/price-list/index.html. Updated September 1, 2020. Accessed August 7, 2020.
- U.S. Department of Health & Human Services. Shingles sends nearly 1 million Americans to the doctor. Accessed at: https://archive.ahrq.gov/news/nn/nn010908.htm. Published January 2008. Accessed August 7, 2020.
- Dworkin RH, White R, O'Connor AB, Hawkins K. Health care expenditure burden of persisting herpes zoster pain. Pain Med. 2008;9(3):348-353.
- Baalbaki NA, Fava JP, Ng M, et al. A community-based survey to assess knowledge, attitudes, beliefs and practices regarding herpes zoster in an urban setting. Infect Dis Ther. 2019;8(4):687-694.
- MacDonald NE; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164.
- Tak CR, Marciniak MW, Savage A, Ozawa S. The essential role of pharmacists facilitating vaccination in older adults: the case of herpes zoster. Hum Vaccin Immunother. 2019:1-6.
- Centers for Disease Control and Prevention. Vaccine Recommendation: a series on standards for adult immunization practice. Accessed at: https://www.cdc.gov/vaccines/hcp/adults/for-practice/standards/recommend.html. May 2016. Accessed August 1, 2020.
- Drug Topics. Making the Shingrix call. Accessed at: https://www.drugtopics.com/view/making-shingrix-call. Published April 20, 2020. Accessed July 15, 2020.
- Centers for Disease Control and Prevention. Vaccines and preventable diseases: administering Shingrix. Accessed at: https://www.cdc.gov/vaccines/vpd/shingles/hcp/shingrix/administering-vaccine.html. Updated January 2018. Accessed July 15, 2020.
Back to Top